Complete electrical isolation of pulmonary veins (PVI) from the left atrium (LA) is crucial to cure patients (pts) with Atrial Fibrillation (AF).1-4
The Cryoballoon catheter ablation technique (CB) has proven effective to achieve this electrical disconnection of pulmonary veins (PV) from LA, resulting in a demonstrated effectiveness to treat pts suffering from PAF.5-11
However, some observations12 have shown, at least when first generation CB was used that cryoenergy CB application doesn’t produce a homogeneous circumferential lesion in all PV, which is related to their anatomical shape, thickness and size with a non-uniform distribution of the atrial muscle around them.
Table 1. Demographic and clinical pts/features
| 128 pts (mean age 53±13) |
| Male/female |
97 (75.8%) / 31 (24.2%) |
| Mean age (male/female) |
58±7 / 61±10 years |
| Mean years/ suffering PAF |
5±5 years (1-5) |
| Mean number/ episodes PAF/ year |
54±67 (2-200) |
| Hypertension |
36 (28%) |
| Diabetes |
6 (4.7%) |
| Structural heart disease |
NONE |
The more elliptic rather than circular variable form at the PV-LA
junction level where cryoenergy is delivered can result in a nonuniform
and persistent cellular lesion which, as is generally accepted,
is the principal cause of PV reconnection after CB ablation.13 A better
quantification of the Cryoablation and the anatomical extent of PV
have been better clarify recently.14 Incomplete lesions with dormant
tissue despite a “perfect” occlusion can occur leading to a residual
conduction (RC) gaps causing, or responsible for PV reconduction
which is the main underlying anatomical substrate for clinical
arrhythmia recurrence.15,16
Adenosine has been used to “unmask” RC in apparently isolated
PV with RF17 and the routine use of AD after acute CB-PVI allows
to identify incomplete lesions with dormant tissue not evident in
basal conditions 18-20 and focal RF applications21 or freeze “touch-up”18-20 eliminate such RC.
The only no evidence of PV/ electrical activity on the circularmapping-
catheter at the LA-PV junction level after CB-PVI is not
enough to assure complete PV-LA electrical disconnection and
checking for entry and exit block is mandatory to confirm it.22-24
We analyzed the seven year follow-up experience of our pts,
initially treated with CB for PAF, with a prospective protocol with
demonstration of complete BB electrical PV-LA-PV block postcryo
and after AD as the main target end point to achieve in all cases.
Since November 2008 to November 2015, a total cohort of 128 pts
(mean age 56±13 years), highly symptomatic, suffering from recurrent
PAF, refractory to medical treatment (Table 1), were treated with the
“CB” and followed-up.
Prior to CB, all pts were previously treated with membrane active antiarrhythmic drugs: Class IC (88.2%); Class III (2.3%); Beta Blockers (BtB) (84.3%) and BtB +1C: 76.5%.
None with structural heart disease. Morphological and structural data can be showed on Table 2:
Exclusion Criteria:
- Prior Stroke, TIA or thromboembolism.
- Cryoglobulinemia and hematological or coagulation disorders.
- Presence of intracavitary thrombi as well as clinically- significant associated comorbidity
Table 2. Morphological and structural LA/PV/LV data
| DIAMETERS
(mm) |
LA |
PV (483) |
LCT (26) |
RCT (3) |
Mean LVEF
67±5% (59-79) |
| AP |
37±6 (21-50) |
18±5 (8-32) |
26±6 (18-35) |
28±1 (27-29) |
| SI |
53±8 (40-75) |
20±4 (10-28) |
26±5 (17-31) |
28±5 (23-33) |
| TR |
46±7 (35-61) |
|
|
|
Mean LA/AREA (cm2)
22±4 (11-32) |
LA: Left Atrium. PV: Pulmonary Vein. LCT: Left Common Trunk. RCT: Right Common Trunk. LVEF: Left Ventricular Ejection Fraction. AP: Antero-Posterior (parasternal long axis). TR: Transversal. SI: Supero-Inferior.
Previous Studies And Anatomical Approach:
2D-Transtoracic
echocardiogram (TTE) as well as, same day, transesophageal
echocardiogram was performed in all cases, to assess cardiac anatomy
and to rule out intramural thrombi.
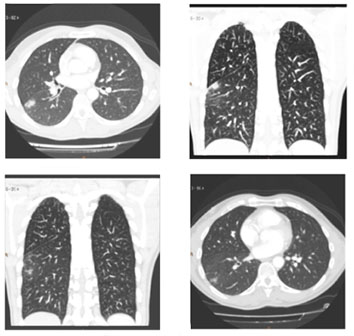
3D/ high resolution/64- slice Multidetector CT scan (Toshiba
Aquilion 64, TSX-101A, Tokyo, Japan), and in some alternative
cases, RMN (1.5T/ Magnetom Symphony, Siemens, Germany)
were used for typification and better definition of cardiac anatomy,
morphology, number, caliber and size of PV in addition to internal
endoluminal navigation analysis to assess the thickness of the
interpulmonary ridge and the morphological shape and size of PV
ostium to choose the optimal CB size and the best orientation to
address the balloon wedging at the LA-PV junction in an attempt
to induce the biggest cryo lesion at the most proximal antral location
including the interpulmonary ridge at the carina level in a sort of
different morphological anatomical variants, as showed in Figure 1.
All pts provided informed consent prior to the procedure.
The procedure was approved by hospital’s clinical ethics committee.
Prior to the procedure, all antiarrhythmic drugs (AAD) were
discontinued at least 5 times their half-life; 48 hours for beta blockers
and at least 10 days for Amiodarone.
All procedures were performed under general anesthesia with
orotracheal intubation under propofol for anesthesia induction,
cisatracurium for neuromuscular relaxation (only at the time of
intubation), continuous perfusion of remifentanil for analgesia and
mechanical ventilation maintained with Sevoflurane gas.
Seldinger technique was used for all vascular
access. A decapolar 6 French electrocatheter through an antecubital
vein was positioned into the coronary sinus (CS) for pacing and
anatomical reference purposes. Cuatripolar/6French catheter was
positioned at the A-V-nodal-his bundle junction through left femoral
vein, for the same anatomical reference purpose, being moved later to
superior vena cava (SVC) for pacing during CB applications at the
right sided PV.
Through right femoral vein, an introducer and fast-cath 8.5 French
sheet SLO, (Saint Jude medical, Minnesota, USA), was advanced over
a 0.32 mm J typed shape guide wire to the SVC. Then, the guide wire is withdrawal, and a modified Brockenbrough needle (BRKO 71 cm
beveled cut 30º/ Saint Jude Medical, MN, USA) is advance through
the SLO sheet, and descending the whole transeptal assembly to
embed fossa ovalis.
Figure 1 Endoluminal and CT Scan reconstruction anatomical approach, to assess diameter/ shape and sizes of PV/LA-PV junction level and interpulmonary ridge, in relation to the size of CB to be used and the orientation for better PV-LA wedging
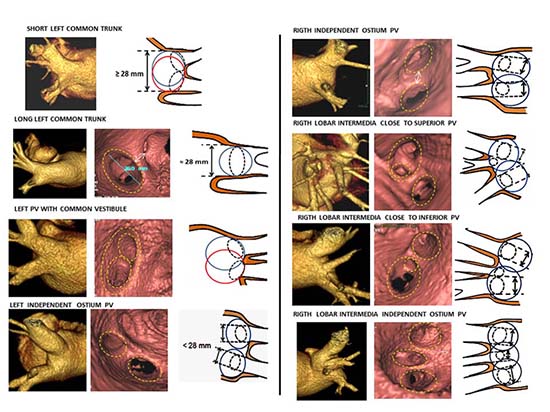
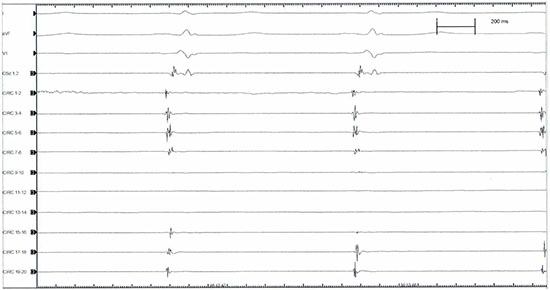
Figure 2A Atrial far-field and synchronous PV electrical activity as recorded with the circular catheter mapping at the PV-LA junction antral level
After gaining left atrial access, a bolus of 10.000 IU of sodium
heparin was administered, followed by continuous perfusion as
needed to maintain the activation clotting time ≥300 sec, as previously
described.25 At the end of the procedure, anticoagulation is reversed
with protamine and 1grm. of lysine acetylsalicylate given i.v, along
with low molecular weight heparine depending on patient’s body
surface (1 mgr/Kg body weight) given subcutaneously, in addition to
100 mg of flecainide given intravenously in 10 minutes. Continuous
intravenous perfusion of sodium heparine adjusted to patient’s body
weight is started 4 hours later after removing all catheters from the
vascular bed. Twenty-four hours later, oral anticoagulation with
Vitamin K antagonist dicumarol is started targeting an international
normalized ratio (INR) in the range of 2.0 to 3.0, plus additional
platelet inhibition with 100 mg of ASA.
Once in the LA chamber, the long
0.32mm guide-wire is advanced into the left superior PV (LSPV)
and selective PV angiogram is performed, and in the same manner for
the remaining veins, Left Inferior (LIPV), Right Superior (RSPV)
and Right Inferior (RIPV).
After removing the entire transeptal assembly, keeping the guidewire
in the LSPV, a steerable 15F over-the wire sheath (Flex Cath,
Cryocath, Medtronic,USA) is advanced and positioned in the LA.
Then basal electrical cartography of the veins is obtained (Figure 2A) with a circular duodecapolar mapping catheter with adjustable
diameter ( Reflexion spiral, Saint Jude Medical, MN, USA)
positioned at the PV-LA junction antrum level, starting on LSPV
and followed by LIPV, RSPV and RIPV respectively. We used a 20
pole circular mapping catheter to achieve sharper signals and better
recognition between PV potentials and far-field atrial activity. This
variable catheter adjustable in diameter is more useful when varying
PV size or common ostium encountered, and also, allows for better
contact and stability at the ostium of the PV when the circular
catheter is fully expanded, leading to relative oversizing. Although,
when fully expanded electrobipoles overlap and could cause contact
signal artifact and repetition of recorded signals.
Figure 2B Asynchronous atrial far-field (Af) and PV electrical potential (PVP) as recorded on circular catheter mapping by pacing CS
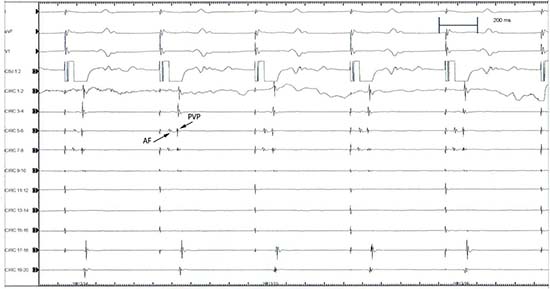
After recording the LA- PV junction electrical activity we pace
CS to separate atrial far-field electrograms from PV electrical activity
Figure 2B, as in sinus rhythm it is difficult to distinguish because they are activated synchronously. After 30 minutes of CB applications
all PVs were mapping again to assess electrical PV-LA isolation.
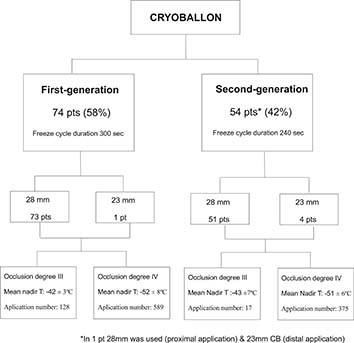
After withdrawing the circular catheter mapping, a 28
or 23 mm double walled CB catheter (Artic Front, Medtronic, USA)
is advanced over the wire up to the LA, inflated and positioned in the
PV ostium of each vein and gently pushed against the PV-LA antrum
to get a perfect occlusion achieved when selective contrast medium
injected (50% ratio with 0.9% saline solution) is full retained into the
vein with no evidence of contrast leakage back to the atrium (grade
IV) according to the degree of occlusion classification proposed and
used by Neumann et al8 to grade I with poor occlusion leading to
an immediate rapid outflow contrast medium back to the LA. Until
the second generation CB (CB2) was commercially available (April,
2013) patients were treated with the first generation CB (CB1).
Bidirectional LA-PV-LA Block Protocol
Exit Block: By pacing PV from all 20 poles of the circular catheter
mapping at high amplitude voltage (20 mA) with consistent 1:1 PV
capture and no evidence whatsoever of any atrial response.
Entry Block: By pacing LA from the CS-Catheter at three
different cycle lengths (600, 500, 400 ms) with consistent 1:1 LA
capture and no evidence whatsoever of any PV electrical activity in
any of the 20 poles of circular-catheter mapping positioned at the
LA-PV junction antral level.
Included bolus i.v administration of increasing doses
(12-18-24… mgrs.), and pacing PV/LA when A-V nodal conduction
block occurred.
Extrapulmonary Muscular Connections (Emc)/ Rule-Out Protocol:
Included pacing distal vein from the circular catheter mapping after
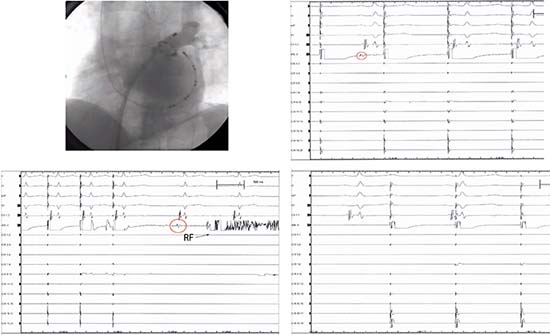
complete BB demonstrated at the LA-PV junction antral level(Figure 4.A)
and the demonstration of 1:1 PV-LA conduction
resumed. (Figure 4.B)
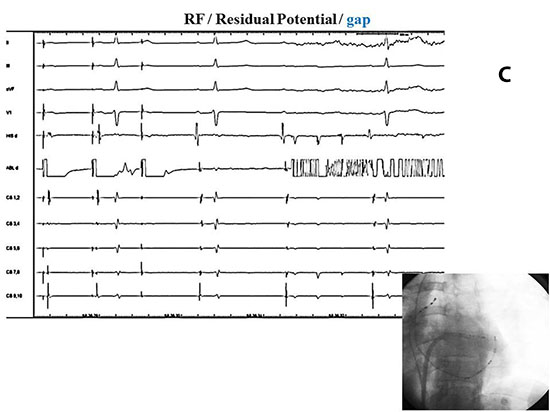
Focal RF applications were used for eliminating RC
gaps when evident after single CB application or after checking for
BB Block, post -AD, or when EMC was demonstrated. (Figure 5).
Sixty second “touch-up” of focal RF was used to eliminate all
residual gaps only when evident in no more than 2 pairs of the
circular catheter mapping. Otherwise, when more a repeated new CB
application was performed.
Figure 3 Diagram flow showing the type of balloon used for different group of pts, occlusion degree, and temperature reached
Phrenic Nerve Physiology Control:
Phrenic nerve physiology was
monitored in all cases during right-sided PV/CB applications, by
placing the cuatripolar electrocatheter in SVC and pacing at 2.000
ms cycle length, checking the intensity of diaphragm contractions by intermittent fluoroscopy and tactile feedback placing the operator’s
hand on the patient´s abdomen, and immediately stop freezing
when intensity of the diaphragm contraction weakens or is suddenly
stopped.
Figure 4 A.Upper panel: Left side: pacing proximal antrum (circular 13-14) showing exit block (right side). B. Lower panel: Left side (same patient): pacing distal vein (circular 13-14), 1:1 PV/LA conduction resumed (right side)
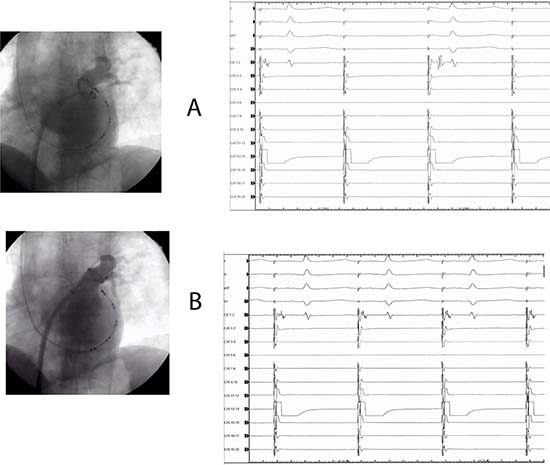
Figure 5 Same patient as figure 4 A, B. Upper panel right side: pacing gap (red circle) distal vein with RF catheter (left side) with: 1:1 PV/LA conduction (third and fourth paced beat) demonstration at the right side recording. Lower panel (left side): pacing gap RF catheter, 1:1 PV/LA conduction is evident (three paced beat). After stop pacing, RC gap is evident (red circle), followed by RF application. After focal RF, exit block is demonstrated (right side)
Before discharge the hospital, TTE was
performed in all cases to rule out pericardial effusion and chest-X-ray
taked in a deep breath, upright position, to confirm normal phrenic
nerve physiology.
The immediate follow-up included holter monitoring at 7,
15,30,45,60 and 90 days respectively, and thorax CT-Scan at 30
and 90 days. All pts received AAD, mostly Class IC+ BtB, and oral
anticoagulation with vitamin K antagonist dicumarol is started 1 day
after PVI, targeting an INR within 2.0 to 3.0 range for at least three
months, along with additional platelet inhibition agent (ASA, 100
mgrs/daily).
After a three-month blanking period on medication, all AAD
were discontinued, and follow-up started to count. All pts were
monitored by continuous daily trans telephonic information in case
of symptoms, and monthly ECG holter monitoring was routinely
done over 1411±727 days (46.6±24.2 months) of follow-up.
Over the last few years, CB ablation technology has emerged into
the arrhythmia arena as an useful and safe tool to treat pts suffering
from atrial fibrillation by achieving through its applications an acute electrical disconnection of the PV from the LA in a range of (90-100
%) in the majority of the series already published,26 which is the main
key to cure this arrhythmia.
Figure 8B Same patient as in Figure A. Upper panel: (left side): pacing (circular 1-2) at PV-LA junction antral level (right side), demonstrated exit block. Lower panel: dormant tissue unmasked by AD (red circle), at the time of complete A-V conduction block, and 1:1 PV-LA conduction demonstrated (second and third paced beats), by pacing gap
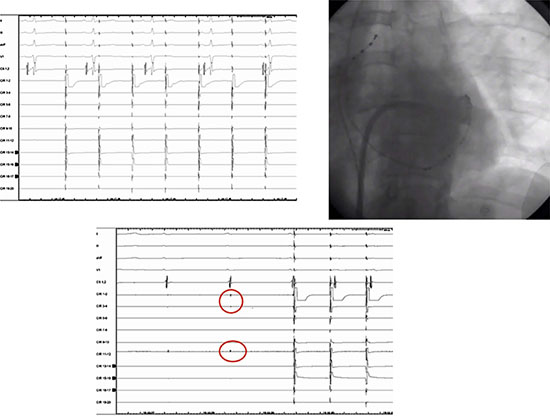
Figure 8C Same patient as in Figure 8A and 8BB. By placing RF catheter (lower right side figure) on PV dormant tissue location unmasked by AD, and pacing gap from RF catheter (upper side recording) 1:1 PV-LA conduction showed on first and second (left side) paced beats during AD effect, as evident with completed A-V conduction block, followed by RF application
Although in the majority of the clinical and randomized studies
published, the results of the CB technique do not significantly differ
in the short, medium and long-term outcome from those using
RF as an energy source,27-30 this “point to point” technique, can be
more tedious, and time-consuming , most likely requiring better
operator skill and involving an inherent clinically-significant risk
of major complications, sometimes difficult to manage and treat,
such as reentry left atrial tachyarrhythmia, thromboembolic events,
pericardial effusion, PV stenosis or atrioesophageal fistula31-34 which
can be avoided or minimizing their incident by a “single shot” CB
technique.
Since the first human experience published by Van Belle et al 5
treating pts suffering PAF with CB ablation, the technique has
become widely-used as useful and safe tool to face the definitive
treatment of this disturbing arrhythmia, by achieving ≥ 95% of acute
electrical PVI in the majority of the series already published.26
Side Effects And Complications:
Figure 9 CT Scan slides showing pulmonary infiltrate (red circles)
Aphonia: We cannot say for certain that this complication was
strictly CB-related, first of all, because as far as we know, it has
not been previously described, which is hardly surprising, especially
after the findings described in the largest survey published so far,35 focusing this complications topic in 500 consecutive pts. Although we
can argue the possibility that this complication has been associated
with endotracheal intubation maneuvers during general anesthesia,
as orotracheal intubation, when difficult, can cause some laryngeal
or vocal chord trauma, this however was not the case regarding our 7
patients affected in whom the orotracheal intubation, was smoothly
performed and non-traumatic. Hence the most logical explanation
for this symptom does not seem to have likely had anything to
do with this orotracheal maneuvers. We raised the question, of
a possible transient injury of the left recurrent laryngeal nerve, as
has been warned by Cabrera and colleagues36 in an unpublished
abstract presentation at Hearth Rhythm 2011meeting, especially
when CB applications take place deeper into the LSPV, along with
the structural displacement towards the anatomical left recurrent
laryngeal nerve bed, by strongly wedging the balloon in the venous
ostium for a better occlusion.
Table 3. Side effects and complications
| TYPE |
Pts |
| Aphonia |
7 (5.4)% |
| Transient Phrenic nerve palsy |
7 (5.4)% |
| Phrenic nerve paralysis |
2 (1.5)% |
| Pulmonary infiltrates |
5 (3.9)% |
| Dyspepsia |
2 (1.5)% |
| Bronchospam |
2 (1.5)% |
| Hemoptoic sputum |
2 (1.5)% |
Moreover, all 7 pts who experienced aphonia were treated with
the CB2 which had been designed with a new technological
implementation resulting in a more homogeneous intake and
distribution of the refrigerant flow around the balloon sphere,
increasing the surface contact cooling that might induce deeper
lesions with greater likelihood of affecting more extracardiac
structures.35,39
PNP occurred in 9 pts (7 %). Only 2 are still permanent after 1
and 3 years follow-up respectively, with not clinical compromise,
doing a normal life and completely asymptomatic. This incidental
complication rate is consistent with the majority of the largest CB
series already published: 4.7%,10-37 7%,5 7.2%,35 7.5%,8 with some
discrete higher incidence 11.1%9 and 11.2%.11
In our series, the common characteristic of this complication was
the lower nadir temperature level reached, of ≤ 60º C in the majority
of cases (78%) Table 4. As the majority of pts were treated with the
CB1 (74 out of 128), the PNP balloon-related rate was: 5.4% CB1
vs 9.2% CB2 (5 pts out of 54). This higher PNP rate occurring with
CB2 as compared to CB1 has been showed by others.38,39 In 340
consecutive pts treated by Aryana et al [38] with CB1 (140) and 200 with CB2, PNP occurred with CB1 in 12.1% pts vs 16.2% when
CB2 was used. In a similar difference percentage rates Fürnkranz
et al39 reported 8.7 % of PNP with CB2 vs 5.7% when CB1 was
employed.
Important to remark in our study that the 2 pts with persistent
PNP after 1 and 3 years of follow-up, PNP occurred suddenly at 100
and 156 seconds of CB1 applications, when the lowest temperatures
of -70 and -68ºC were respectively reached. In the other 7 pts with
transient PNP, the CB applications were immediately stopped as soon
as weakness of the diaphragm intensity contraction was adverted.
Table 4. Ocurrence of PNP related to the CB used, time of application and nadir temperature reached
|
TºC |
Seconds |
CB mm |
CB Generation |
78%
Mean TºC≥
-60ºC
|
| 1
|
-68 |
122 |
28 |
FIRST |
|
| 2 |
-73 |
222 |
28 |
FIRST |
|
| 3 |
-55 |
89 |
28 |
SECOND |
First Gen CB: 55.5% |
| 4 |
-56 |
165 |
23 |
SECOND |
|
| 5 |
-60 |
115 |
28 |
SECOND |
|
| 6
|
-68 |
100 |
28 |
SECOND |
|
| 7 |
-65 |
190 |
28 |
SECOND |
Second Gen CB: 45.5% |
| PERMANENT PHRENIC NERVE PARALYSIS |
|
|
|
|
|
| 1
|
-70 |
100 |
28 |
FIRST |
|
| 2 |
-68 |
156 |
28 |
FIRST |
|
TRANSIENT PHRENIC NERVE PALSY
The highest level of PNP (19%) reached with the CB2 observed by Cherchia et al 40 related with the lower CB temperature reached,
has move to this group to stop CB applications when -60 º C
nadir temperature level is reached, in addition to limiting the
freeze application time to 180 seconds, in an attempt to avoid
major complications.41,42,35 At the same time, these authors have
proposed a modification technique to prevent PNP, consisting
after tight wedging of the inflated CB inside the RSPV ostium,
to withdraw it until a small leak of contrast is observed, since the
CB volume increases slightly at the onset of CB application. This
technical maneuvers described by Casado-Arroyo et al43 from the
same Brussel’s group, offers the advantage of a more proximal CB
application and it has been suggested to use by others.44 Martins et al
suggest the use of Casado-Arroyo technique, particularly when the
vertical projection of the PN reaches the distal part of the CB (Zone
B1 in their study) with a 98% of negative predictive value, and Ströker
et al 45 had recently emphasized the need to perform a preprocedural
anatomic assessment, in order to evaluate the risk of PN injury, such
PV orientation, larger PV dimensions, shorter distance to SVC, the
presence of early branches originating from the main ostium, and
right –sided long CT; anatomical variations which were associated
with PN injury.
Pulmonary Infiltrates: Of unknown origin, mostly showed on
the right side in distal pleural location, found in 5 asymptomatic
pts (3.9%) on CT-Scan control routinely performed 1 month after
the procedure, which were no longer evident at the 3-month control
CT-Scan performed, at follow-up. Those pulmonary infiltrates,
radiologicaly in appearance of inflammatory aspect, producing no
clinical impact on pts, strongly suggest a probably origin related
with the transmission of cold into the lung parenchyma during CB
application, as it has been experimentally demonstrated in dogs46 as
small subtle foci of ablated –related superficial pleural fibrosis.47
Severe intraprocedural bronchospasm occurred in two pts who had a past medical history of mild chronic bronchitis
whom required medical treatment for ≤ 48 hours in the ICU. This
complication might have a difficult explanation and could have been
due to a combination of several factors working together, such as
prior bronchial damage in pts with chronic bronchitis, the possibility
of major injury due to ice formation inside the bronchial lumen48 as
well as the possible trigger effect of AD which, although anecdotic,
has been described.49
Hemoptoic Sputum: Two pts presented discrete hemoptoic
sputum on the immediate post- procedure, being otherwise on oral
anticoagulation treatment regime and completely asymptomatic.
This type of complication might also be due to several factors
working together or may even have a different origin. Firstly, as it has
been experimentally demonstrated,50,51 the expansion of ice within
the fragile microvasculature leads to the interruption of vascular
integrity, which is the reason for the intramyocardial hemorrhage,
as well as the hemoptysis associate with cryo injury to the lung
tissues, and secondly, the possibility of bronchial erosion as has been
demonstrated52 as a cause of hemoptysis.
Dyspepsia: Two pts complain of mild dyspepsia. As no
esophagogastroduodenal endoscopy study was performed, we
cannot assure it was related or not, with some reversible esophageal
ulceration.53
Epicardial PV-LA muscular connections: Electrically functioning
EMC with PV-LA 1:1 conduction Figure 4 A, Figure 4 B demonstrated,
was found in our pts using this protocol in 12 PV (2.5% of total 483
PV), totaling 27.2% of the all post CB- PV reconducted (44 PV),
in 9 pts (7%).
Since the first human demonstration of the presence of electrical
conduction between PV was made,54 other investigators had
demonstrated the incidence of the interpulmonary vein electrical
connections as being responsible of the maintenance of the arrhythmia
in a single pt with PAF,55,56 and Takahashi et al demonstrated in
49 consecutive pts, the presence of electrical connections between
contiguous PV in 14% of the pts underwent atrial RF catheter
ablation to treat their drug-resistant AF.57
Perez- Castellano et al58 using RF catheter ablation for ostial PVI
in 100 consecutive pts with drug-refractory atrial fibrillation, found in
3% of the veins, venoatrial epicardial connections inserted at distance
from the venous ostium, and 10% with epicardial connections
between the ipsilateral PV in 20% of pts resistant to atrial ablation,
suggesting a different disconnection approach for PV showing those
extrapulmonary epicardial connections associated with an increased
rate of early recurrence of conduction.
The morphological evidence of these muscular connections
between contiguous veins has been demonstrated by Cabrera et al,59
confirming the anatomical underlying substrate of such electricallyfunctioning
connections. More recently, Squara et al60 have
demonstrated the prevalence of those electrical connections between
ipsilateral pulmonary veins and their implications for ablation and
AD testing in 30 pts submitted to RF catheter ablation. They found
a high presence of ipsilateral PV connections after antral PVI in up
to 65.6% of total PV sets without carina ablation, lowered to 17.7%
when the carina ablation was performed, emphasizing the need for
carina ablation. Squara et al 60 also described acute reconnection of at
least 1 of the PV to the LA, in 18% of the PV sets.
In our work 44 PV (9.1%) of the total PV faced (483) showed acute
reconduction after single CB Figure 6.As we have not conducted any previous study to assess the prevalence of these possible direct
connections between ipsilateral pulmonary veins, and quantifying
the incidence rate that the electrical impulse originating from 1 PV
would propagate to the adjacent ipsilateral vein, as well as the indirect
connections LA muscular sleeves, the only way to demonstrated
some EMC in a practical clinical setting is the demonstration of
complete BB at the PV-LA junction antral level by pacing from
all 10 pairs of poles of the duodecapolar circular catheter mapping,
following by demonstration that 1:1 PV-LA conduction resumed
by pacing distal vein Figure 4 A, Figure 4 B no further than 5-10mm from
the endocardium of the interpulmonary isthmus, as Cabrera et al59
have demonstrated as the limit of distance where the insertion of the
muscular connections, can be founded.
By doing so, we found electrically -functioning EMC in 12 (2.5%)
of the total PV-LA reconnected after CB-PVI, totaling 27% of the
all early- reconducted veins, which is consistent with the figures
published by others,58 having carried out the same protocol, to ruleout
EMC, by pacing distal vein after PVI-atrial isolation. Another
interesting aspect to be taken in account is that, in the majority of
CB-applications the interpulmonary ridge of the PV isthmus at the
carina level is, affected, regardless of PV anatomy, (except for long
CT) affected by cryo lesion at the endocardial superior and inferior
aspects during CB applications at the superior and inferior PV.
Interestingly, those 12 EMC were demonstrated after acute BB
was achieved in 9 pts, totaling a 7% of the total population of pts
treated.
AD Protocol And Acute Early PV-LA Reconnection:
A total of
483 PV including 29 CT were treated with CB and complete CBPVI
demonstrated in 439 (90.9%). Acute reconduction post CB was
PV; 36% of the reconducted ones), show acute reconnection due to
incomplete lesion with “dormant tissue” unmasked by AD,17,18 by
inducing hyperpolarization to restore excitability by activating ADsensitive
potassium channels restoring conduction of dormant PV as
it has been better clarified and demonstrated by Datino et al61
Arrhythmia Recurrence And Reconduction:
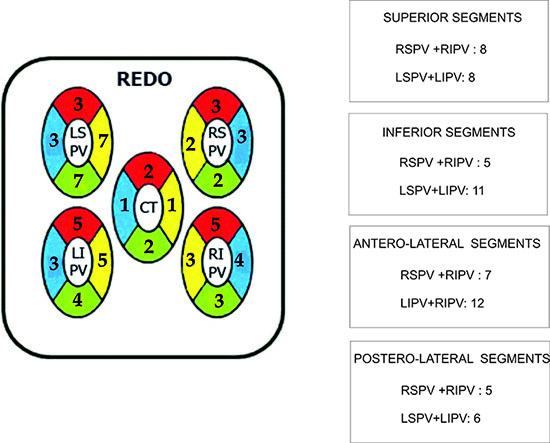
For analysis of the
location of conduction gaps, the ipsilateral LA-PV junction was
divided into four segments in a clockwise sense, starting at 10 o’clock
(Superior, inferior, anterior, and posterior, for left PVs, and superior,
inferior, septal, and lateral, for right PVs ) Figure 10.
Figure 10 Diagram representation for the different number of RC found in the different segment location
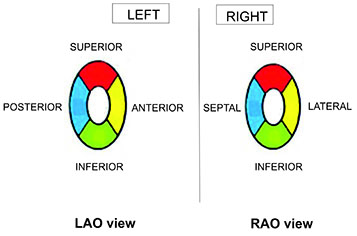
Forteen pts (10.9%) had clinical recurrence of the arrhythmia and allow for a Redo. Fifty-four PV including 2 CT were newly CB
treated in a Redo with CB2. Reconduction was encountered in 29
PV (53.7%) in different segment locations Figure 10_A revealing
the almost even distribution of RC in the superior segments, with
greater number of reconductions shown at the inferior aspect of the
LSPV. Also the PV showing the largest number of reconduction was
the LSPV (37.9%) Table 5.
Finally, the RC segment distribution on Redo cases was random,
being unrelated to those shown at first procedure Figure 10_B.
Fürnkranz et al 15 find the inferior segments of the LA-PV junction
most often affected by reconduction in addition to the LSPV having
shown the high rate of reconduction (63%), suggesting that the
superior ridge may have contributed to this relatively high rate of
reconduction in this LSPV.
In addition to the above, Fürnkranz et al hypothesized in their
aforementioned study that the high incidence of inferior conduction
gaps might be due to different causes, related to the difficulty
sometimes involves in deflecting the sheath/balloon system in order
to reach the inferior aspect of PV, resulting in incomplete balloontime
contact. Conversely when approaching superior PV, both
sheaths and balloon can be used to create a strong push onto the
PV ostium to occlude the blood flow, achieving better occlusion and
more permanent tissue cryolesion.
In the original study conducted by Chierchia et al,19 enrolling 39
pts treated for PAF with CB1, AD testing after CB induced a LAPV
reconnection only in 7 (4.6%) PV which often occurred in the
inferior aspect of the lower veins, especially of the right inferior. All
these RC gaps being eliminated by further CB applications or focal
cryo “Touch-up”. Chierchia et al,16 have also shown a 2.8% early
spontaneous reconnection after 30 minutes of CB applications in a
cohort of 26 pts treated for PAF with CB1.More recentlyin a study
conducted by Ciconte et al 20 in 50 consecutive pts treated for PAF
or early persistent AF ≤ 6 months, with CB2, spontaneous (4 veins)
and AD-induced (4 veins) PV reconnections occurred in the 4% of
initially isolated veins (8 veins) in 6 pts (12%).
Our results are consistent with the aforementioned studies, entailing
36% totally reconnected PV showing spontaneous reconduction,
totaling 3.3% of the total 483PV-CB treated. Beside the highest
reconduction gaps on the inferior aspect of the LSPV, conversely to
the segment location reconduction showed by Fürnkranz et al15 in
26 pts refered for RF PV ablation after CB first procedure failed,
inferior segments showed gaps in 85% and 77% at the lateral and
septal location respectively and 42% and 31% respectively at the
lateral and septal aspect of the superior segments, our segment
reconduction locations showed a most uniform distribution.
Table 5. Number of PV showing reconduction and their percentages of the total PV reconnected
| PV |
nº |
% |
| CT |
2 |
6,8% |
| LSPV |
11 |
37,9% |
| LIPV |
7 |
24,1% |
| RSPV |
4 |
13,7% |
| RIPV |
5 |
17,2% |
14 pts: 54 PV (2CT)
One possible underlying explanation for this, perhaps being the fact that in our pts all procedures were performed by the same
operator (JMP) and were evaluated individually case by case, based
not only the size of balloon to be used, but also on the orientation
to be applied15 according to PV anatomy, morphology, and angle
direction, previously assessed with CT-PV slide reconstructions,
in conjunction with the aforementioned endoluminal anatomical
approach Figure 1. All of these factors combined might play an
important role toward achieving better occlusions and more uniform
lesions adding to minimize possibilities of PV-LA reconduction,
which is the principal cause of clinical arrhythmia recurrences.
Figure 10A Segment distribution appearance of RC gaps
We have not done any protocol to rule out non PV-Foci, as a
potential cause of arrhythmia recurrence,62 given that all recurrences
were Redo, and PV-LA reconduction was evidenced in all cases.