Structured care of patients with atrial fibrillation improves guideline adherence
Neshro Barmano1,2,3, Ulla Walfridsson2,4, Håkan Walfridsson2,4, Jan-Erik Karlsson11,2,3
1Department of Internal Medicine, County hospital Ryhov, Jönköping, Sweden.2Department of Medical and Health Sciences, Linköping University, Linköping, Sweden.3Jönköping Academy, Jönköping University,Jönköping, Sweden and.4Department of Cardiology, University hospital, Linköping, Sweden.
There are many reports of lack of guideline adherence in the treatment of patients with atrial fibrillation (AF), and AF affects health-related quality of life (HRQoL) negatively. The aim of this study was to investigate whether structured care compared to standard care of a general AF population could improve guideline adherence and HRQoL, and reduce symptoms,anxiety and depression.
In total, 176 patients were recruited to the intervention and 146 patients to the control group.The intervention consisted of a structured follow-up program, while patients serving as controls received standard care. The primary outcome was guideline adherence evaluated through: appropriate use of oral anticoagulants (OAC) and antiarrhythmics, whether echocardiogram and thyroid lab tests were performed, and patient-reported outcome measures (PROMs), assessed with the questionnaires SF-36, EQ-5D, HADS and ASTA at baseline and after one year.
Guideline adherence was significantly better in the intervention group, 91% vs. 63% (p < 0.01), mainly due to appropriate OAC treatment 94% vs. 74% (p < 0.01). Symptoms assessed with ASTA were less frequent and the negative impact of AF was reduced in the intervention group after one year/ at follow-up. Five scales in SF-36, and the visual analogue scale for current health status in EQ-5D (EQ-VAS), improved significantly in both groups.
Structured care of patients with AF significantly improved guideline adherence and patients reported fewer symptoms and a reduced negative impact on disease-specific HRQoL compared to standard care at one year follow-up.
Key Words : Atrial fibrillation, Guideline Adherence, Anticoagulants, Health-related Quality of life, Symptoms, Anxiety.
Correspondence to: Address reprint request to Dr. Barmano, Department of Internal Medicine, County Hospital Ryhov, SE-551 85 Jönköping, Sweden
Atrial fibrillation (AF) is the most common cardiac arrhythmia with a prevalence of approximately 3% in the Swedish population, and increases with age[1]. Due to an aging population, the number of patients with AF will increase, which implies great demands on the healthcare services. AF is associated with heart failure, disabling symptoms, decreased health-related quality of life (HRQoL), increased mortality and risk of ischaemic stroke[2].Approximately 15% of all strokes are due to AF and among octogenarians as many as 25%[3]. Ischaemic stroke due to AF leads to higher mortality and greater disability than a stroke caused by other reasons[3]. Although it is well-known that treatment with oral anticoagulants (OAC) in high risk patients significantly reduces the risk for stroke, there are many reports of its underuse[4]. Studies have shown that other factors than well-known risk factors for stroke are often involved in the decision on whether to prescribe OAC or not[4].There is a lack in guideline adherence in other areas as well, especially echocardiography[5].
Secondary to stroke prevention, the care of patients with AF should focus on symptom relief and improvement in HRQoL, since AF often leads to more or less severe symptoms and a reduced HRQoL[6]. Anxiety and depression are particularly strong predictors of HRQoL in patients with AF[6], [7]. Symptoms, anxiety, depression and HRQoL can be evaluated by patient-reported outcome measures (PROMs). PROMs provide a way to gain insight into how patients perceive their health and offer a way to measure the effects of healthcare interventions, most commonly through self-completed questionnaires[8].
The aim of this study was to investigate whether structured care compared to standard care of a general AF-population could improve guideline adherence and HRQoL and decrease symptoms, anxiety and depression.
The study had a non-randomised prospective design. The intervention took place at the Ryhov county hospital in Jönköping, Sweden, while patients in the control group were enrolled at three county hospitals in the same area (Kalmar, Eksjö and Norrköping, Sweden). All patients were asked to fill out questionnaires at inclusion and after one year, and their medical records were examined one year after inclusion. There was no study-related contact with patients in the control group, while patients in the intervention group were followed at the AF clinic as described below. Educational level, occupation and cohabitation was registered. The first patient was included in December 2009 and the last follow-up was made in April 2014.Ethical approval was obtained from the Regional Ethical Committee in Linköping (Dnr. M145-09). The study complies with the declaration of Helsinki.
All patients ≥ 18 years who visited the emergency room (ER) due to AF were eligible for participation. Written informed consent was obtained prior to enrolment. Exclusion criteria were unwillingness to participate, unstable coronary artery disease, sepsis or other severe infection, AF early after thoracic surgery, acute pulmonary embolism, known hyperthyroidism, malignant disease with expected survival less than one year, dementia or insufficient knowledge of the Swedish language making it difficult to independently fill out the questionnaires.
In 2006, a survey of the population in south-eastern Sweden was conducted, including assessment of HRQoL measured with, among others, SF-36. In total, 7 238 individuals responded to the survey, and the individuals aged 65-74 years were used for comparison.
Eligible patients were informed of the study at the ER or at the cardiac ward. Enrolled patients were then scheduled for an outpatient visit at the AF outpatient clinic (see below) within two weeks. Patients enrolled at the hospitals serving as control centres were only asked to fill out the questionnaires and then received ”care as usual”.
Structured care of atrial fibrillationEducation and preparations
Prior to study onset, physicians at the emergency care unit at the intervention centre were educated concerning current guidelines. A pocket sized laminated algorithm was presented, containing recommendations for treatment with oral anticoagulants (OAC) and with suggestions for outpatient management.
Atrial fibrillation outpatient clinic
The AF outpatient clinic was active one day weekly and manned by two cardiologists and two nurses. All patients included in the study were followed at the AF outpatient clinic for one or two weeks after discharge and then after three and 12 months. Data was entered in the Swedish National quality AF registry (Auricula) at the first and last visits. The nurses` perspective was information and education in order to increase the patients’ knowledge about AF. They also provided information on lifestyle with focus on overweight/obesity, the amount of alcohol and coffee use, stress and psychological distress. In addition to the orally given information, an information booklet from the Swedish Heart and Lung Foundation was handed out, containing general information about AF including basic anatomy,physiology,symptoms and treatment. The physician’s evaluation was made aided by a checklist to ensure that treatment was given according to guidelines. If OAC was not prescribed when indicated,an explanation was mandatory. Increased availability was also a part of the structured AF outpatient clinic. Patients could reach a nurse every weekday morning.
The primary outcomes were the effect of structured care on guideline adherence, symptoms, anxiety, depression and HRQoL. Adherence to guidelines was evaluated by five criteria: a) appropriate prescription of OAC according to the CHADS2 and CHA2DS2-VASc criteria ([Table 1]), b) echocardiogram performed, c) thyroid laboratory tests performed, d) no antiarrhythmic drugs (AA) prescribed to patients in permanent AF, and e) no class 1c-AA prescribed in the presence of structural heart disease. At the onset, the recommendation in the guidelines were based upon the CHADS2 classification scheme and suggested the use of OAC when CHADS2 ≥2 in patients without contraindications. During the study, new guidelines were published recommending the use of the CHA2DS2-VASc classification scheme and treatment with OAC for scores ≥1. Symptoms, anxiety, depression and HRQoL were assessed by the following questionnaires:
Table 1. The CHADS2, CHA2DS2-VASc-score and annual stroke risk.
|
Risk factor
|
Score in the CHADS2a scheme
|
Score in the CHA2DS2-VAScb scheme
|
|
Congestive heart failure/LV dysfunction
|
1
|
1
|
|
Hypertension
|
1
|
1
|
|
Age > 75
|
1
|
2
|
|
Diabetes mellitus
|
1
|
1
|
|
Stroke/TIA/thrombo-embolism
|
2
|
2
|
|
Vascular disease
|
-
|
1
|
|
Age 65-74
|
-
|
1
|
|
Sex category (i.e. female sex)
|
-
|
1
|
|
Maximum score
|
6
|
9
|
.
|
Total score
|
Adjusted stroke rate (%/year) according to CHADS2-score
|
Adjusted stroke rate (%/year) according to CHA2DS2-VASc-score
|
|
0
|
1.9
|
0
|
|
1
|
2.8
|
1.3
|
|
2
|
4.0
|
2.2
|
|
3
|
5.9
|
3.2
|
|
4
|
8.5
|
4.0
|
|
5
|
12.5
|
6.7
|
|
6
|
18.2
|
9.8
|
|
7
|
|
9.6
|
|
8
|
|
6.7
|
|
9
|
|
15.2
|
aCHADS2-score is a stroke risk classification scheme, using a point system ranging from zero to six. Presence of congestive heart failure, hypertension, age 75 years or above and diabetes give one point each, and previous stroke/TIA or other arterial embolism give two points. bCHA2DS2-VASc-score is an extension of the CHADS2-score, adding the risk factors vascular disease and female sex. Furthermore, age 65 years or above gives one point, and 75 years or above two points. The summed score ranges from zero to nine points. LV, left ventricle; TIA, transient ischaemic attack
The Medical Outcomes Study 36-Item Short-Form Health Survey
The Medical Outcomes Study (MOS) 36-Item Short-Form Health Survey (SF-36) is a generic questionnaire designed to measure an individual’s physical and mental health. It comprises 35 items grouped into eight scales and one question concerning changes in health outside the scales. The eight scales are physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE), and mental health (MH). For each of the eight scales scores were coded, summed, and transformed to a scale from 0 (worst possible health) to 100 (best possible health). The scoring of the SF-36 data was carried out as described by Ware and colleagues[9]. SF-36 has been widely used in research, including studies of patients with arrhythmias[6], [10].
The EuroQol Health Questionnaire, five dimensions and EuroQol Health Questionnaire,Visual Analog Scale
The EuroQol Health Questionnaire, five dimensions (EQ-5D) and EuroQol Health Questionnaire, Visual Analog Scale (EQ-VAS) questionnaire was used to characterize health state. The EQ-5D questionnaire assesses five dimensions; patient mobility, self-care, activity, pain/discomfort, and mood, each with three levels of severity. The UK EQ-5D index tariff was used to obtain a weighted index, with a range from -0.59 to 1.0, where 1.0 represents full health[11]. The EQ-VAS records the respondents’ self-rated health status on a vertically graduated (0–100) visual analogue scale with 100 (best imaginable health state) at the top and 0 (worst imaginable health state) at the bottom. EQ-5D/EQ-VAS has been extensively validated and is one of the most used generic HRQoL instruments in AF studies [10].
The Hospital Anxiety and Depression Scale
The domain specific questionnaire Hospital Anxiety and Depression Scale (HADS) is used to evaluate symptoms of anxiety and depression. It consists of two subscales, where seven questions assess anxiety (HADS-A) and the remaining seven assess depression (HADS-D).Responses are scored from 0 to 3 with higher scores denoting more psychological distress.The score for each subscale can range from 0 to 21. The scores are categorized as normal (0-7), mild (8-10), moderate (11-14) and severe (15-21) anxiety and/or depression respectively[12]. HADS has previously been used in AF studies[13].
The Arrhythmia-Specific questionnaire in Tachycardia and Arrhythmia
The disease-specific Arrhythmia-Specific questionnaire in Tachycardia and Arrhythmia (ASTA) is divided into three separate parts where part I evaluates the patient’s latest episode of arrhythmia, current medication and the patients’ subjective feeling of any existence of arrhythmia. Part II evaluates symptom burden including frequency and duration of arrhythmia episodes, and contains a 10-item symptom scale with four response alternatives: “(0) No, (1)Yes, to a certain extent, (2) Yes, quite a lot and (3) Yes, a lot. Outside of the Symptom scale there are two questions concerning “near syncope” and “syncope” with the response alternatives Yes/No. Part III assesses the influence on HRQoL and consists of a 13-item scale with seven physical subscale items and six mental subscale items. The response alternatives are the same as for the symptom scale in part II[14], [15]. In order to evaluate experiences of achieved freedom from arrhythmia-specific symptoms and negatively influenced HRQoL after one year , the variables were dichotomized to the responses “Yes” or “No”.
In order to detect a five-point difference in the scales in SF-36 between the groups using an alpha of 0.05 and a power of 0.80, 200 patients in each group were required. Normally distributed variables are presented as means ± standard deviations, whereas categorical variables are presented as percentages and numbers. Differences between the two patient groups for normally distributed variables were tested with independent t-test, and paired t-test for differences over time within the groups. For non-normally distributed variables the Mann-Whitney U test was used for testing differences between two groups, and Wilcoxon’s signed rank test within groups over time and McNemar’s test was used for dichotomous variables. For categorical variables the Chi-square test or Fischer’s exact test were used between groups, and for proportions the z-test with continuity correction was used. All calculations were made with SPSS statistical software version 20.0 (Armonk, NY: IBM Corp). P-values <0.05 were considered as statistically significant.
The intervention group consisted of 199 patients and the control group of 162, and patients available for analysis were 176 (88%) and 146 (90%), respectively. ([Figure 1]). The two groups differed at baseline concerning educational degree, number of patients with CHADS2 0 p, and the number of patients having their first episode of AF ([Table 2]).
Figure 1. Study inclusion flowchart
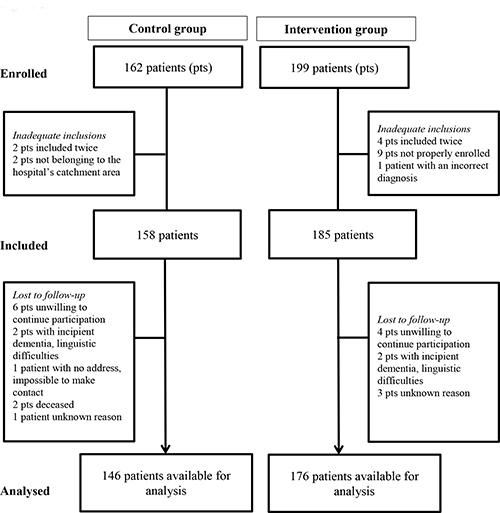
Table 2. Baseline characteristics
|
Characteristics
|
Intervention group (n = 176)
|
Control group (n = 146)
|
p-value
|
|
Age years, mean +- SD
|
66 +- 10
|
68 +- 11
|
0.06
|
|
Male gender, no. (%)
|
112 (64)
|
84 (58)
|
0.26
|
|
Type of AF, no. (%)
|
|
|
0.12
|
|
First episode
|
42 (24)
|
50 (35)
|
< 0.05*
|
|
Paroxysmal
|
62 (35)
|
49 (34)
|
Ns.
|
|
Persistent
|
57 (32)
|
38 (26)
|
Ns.
|
|
Permanent
|
15 (9)
|
7 (5)
|
Ns.
|
|
Comorbidity, no. (%)
|
|
|
|
|
Hypertension
|
81 (46)
|
79 (54)
|
0.13
|
|
Diabetes
|
13 (7)
|
20 (14)
|
0.06
|
|
Ischaemic heart disease
|
21 (12)
|
24 (17)
|
0.34
|
|
Congestive heart failure
|
23 (13)
|
14 (10)
|
0.28
|
|
Chronic pulmonary disease
|
10 (6)
|
5 (3)
|
0.42
|
|
Previous Stroke/TIA
|
11 (6)
|
15 (10)
|
0.15
|
|
CHADS2-score no. (%)
|
n = 176
|
n = 143
|
0.09
|
|
0*
|
70 (40)
|
40 (28)
|
< 0.05*
|
|
1
|
57 (32)
|
57 (40)
|
Ns.
|
|
> 2
|
49 (28)
|
46 (32)
|
Ns.
|
|
CHA2DS2-VASc-score, no. (%)
|
|
|
0.16
|
|
0
|
30 (17)
|
15 (11)
|
Ns.
|
|
1
|
40 (23)
|
29 (20)
|
Ns.
|
|
> 2
|
106 (60)
|
99 (69)
|
Ns.
|
|
OAC when indicated, no. (%)
|
|
|
|
|
CHADS2 > 2
|
24 (65)
|
17 (63)
|
Ns.
|
|
CHA2DS2-VASc > 2
|
44 (60)
|
34 (60)
|
Ns.
|
|
CHADS2 > 1
|
42 (58)
|
35 (55)
|
Ns.
|
|
CHA2DS2-VASc > 1
|
51 (61)
|
42 (55)
|
Ns.
|
|
Cohabitation, no. (%)
|
n = 176
|
n = 123
|
0.90
|
|
Living alone
|
39 (22)
|
28 (23)
|
Ns.
|
|
Living with partner and/or child
|
137 (78)
|
95 (77)
|
Ns.
|
|
Educational level no. (%)
|
n = 171
|
n = 124
|
0.02+
|
|
Primary school*
|
66 (38.6)
|
68 (55)
|
< 0.05*
|
|
High school
|
56 (32.7)
|
31 (25)
|
Ns.
|
|
University
|
49 (28.7)
|
25 (20)
|
Ns.
|
|
Occupation no. (%)
|
n =176
|
n = 120
|
0.32
|
|
Employed
|
58 (33)
|
33 (27.5)
|
Ns.
|
|
Unemployed/age retirement
|
118 (67)
|
87 (72.5)
|
Ns.
|
* p < 0.05 for the proportion between the study groups, by calculating the z score with continuity correction †p < 0.05 for the variable between the study groups, analysed with Chi2-test Cursive letters in the last column indicate significant (p < 0.05) or non-significant (ns.) p-values by calculating the z score with continuity correction AF, atrial fibrillation; OAC, Oral anticoagulants; SD, standard deviation; CHADS2, congestive heart failure, hypertension, age ≥ 75, diabetes, stroke; CHA2DS2-VASc, congestive heart failure, hypertension, age ≥ 75, diabetes, stroke, vascular disease, age 65-74 years, sex category (i.e. female sex); Ns., Non-significant
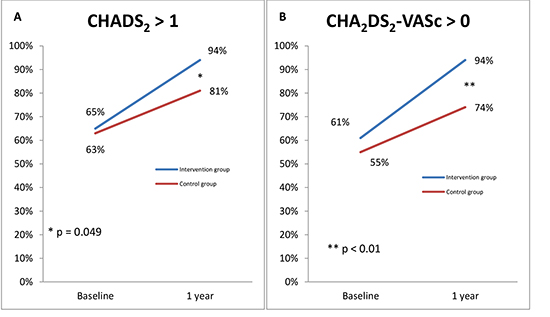
At baseline, there was no difference in treatment with OAC according to guidelines between the intervention group and the control group, 27 (65 %) vs. 17 (63 %, p = 0.88) using CHADS2, and 51 (61 %) vs. 42 (55%, p = 0.43) using CHA2DS2-VASc. The number of patients treated according to guidelines after one year, in terms of adherence to all five criteria investigated, was significantly better in the intervention group, 152 (93%) vs. 105 (74%, p < 0.01). The difference in total adherence to guidelines was greater using the CHA2DS2-VASc in favour of the intervention group after one year, 148 (91%) vs. 89 (63%, p < 0.01). This was mainly due to an improvement in OAC treatment ([figure 2]). There were also significant differences in whether thyroid function was tested or not, 175 (99%) vs. 126 (86%, p < 0.01). However, there were no differences in investigations with echocardiogram, 164 (93%) vs. 133 (92%, p = 0.62), in whether patients were treated with AA although in permanent AF (none in both groups), or whether a class Ic-AA drug was used despite presence of structural heart disease (two patients in each group).
Figure 2. The proportion of patients in the intervention and control groups treated with oral anticoagulation (OAC) according to guidelines using the CHADS2-criteria (A) and the CHA2DS2-VASc-criteria (B) at baseline and at follow-up after one year.
During follow-up, stroke, transient ischemic attack or peripheral embolus occurred in five patients (3%) in the intervention group and three patients (2%) in the control group. Two patients in the intervention group suffered from intracerebral bleeding, while one patient in the intervention group and one patient in the control group suffered from gastrointestinal bleeding.
The number of patients with CHA2DS2-VASc 0 p after one year was 21 (12 %) and 11 (8 %) in the intervention group and control group, respectively. However, seven (33 %) and five (46 %) of those patients were treated with OAC (n.s.) and the reasons were recent or planned ablation or DC-conversion, patients’ own will to continue, close to reaching 65 years of age and in one patient a second echocardiography was planned since the left ventricular function was hard to evaluate due to arrhythmia in the first echocardiography.
Patient-reported outcome measures
The number of enrolled patients that did not return the questionnaires at follow-up was seven (4%) in the intervention group and 48 (33%) in the control group. There were also a number of missing answers within the questionnaires, hence the numbers of patients not included in the analyses of PROMs were greater for some scales.
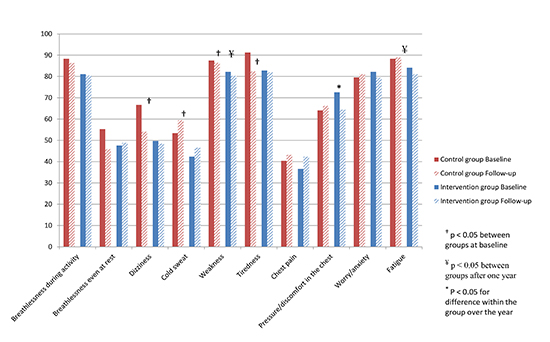
Compared to the intervention group, patients in the control group reported more dizziness (p =0.01), cold sweat (p = 0.03), weakness (p = 0.02) and tiredness (p = 0.04) at baseline, and after one year more weakness (p = 0.04) and fatigue (p = 0.03), as assessed with ASTA. Over the year, significantly fewer patients were feeling pressure in the chest in the intervention group ([figure 3]) while no significant change was seen in the control group.
Figure 3. Percentage of patients with any degree of symptoms, assessed with the Arrhythmia-Specific questionnaire in Tachycardia and Arrhythmia (ASTA) at baseline and after one year in the control and the intervention groups.
The degree of anxiety assessed with HADS was normal at baseline, e.g. ≤7 in 120 (75 %) patients in the intervention group and in 96 (79 %) patients in the control group. The degree of depression was normal in 128 (81%) and 106 (86 %) patients, in the intervention group and control group, respectively. There were no significant differences between the groups.
The degree of anxiety was reduced after one year in both groups, while depression did not change significantly ([table 3]). The scoring did not differ between the groups at the one year follow-up.
Table 3. Health-related quality of life, anxiety and depression scores at baseline and after 1 year, and statistical analyses of differences between the groups and within the groups over the year
|
Questionnaire
|
Group
|
Baseline, mean +- SD
|
1 year, mean
+- SD
|
Changes over the year, mean +- SD
|
Difference between groups at baseline (p-value)
|
Difference between groups after 1 year (p-value)
|
Difference between groups over time (p-value)
|
Difference within groups over time (p-value)
|
|
SF-36
|
|
|
|
|
|
|
|
|
|
PF
|
Intervention
Control
|
73 +- 23
63 +- 27
|
71 +- 25
70 +- 24
|
-1 +- 17
2 +- 17
|
<0.01**
|
0.54
|
0.12
|
0.48
0.17
|
|
RP
|
Intervention
Control
|
45 +- 44
35 +- 42
|
62 +- 44
52 +- 44
|
17 +- 48
15 +- 43
|
0.04*
|
0.07
|
0.75
|
<0.01**
<0.01**
|
|
BP
|
Intervention
Control
|
68 +- 28
65 +- 27
|
71 +- 26
66 +- 28
|
2 +- 26
0 +- 29
|
0.29
|
0.21
|
0.63
|
0.29
0.87
|
|
GH
|
Intervention
Control
|
58 +- 20
55 +- 20
|
60 +- 21
56 +- 22
|
3 +- 17
0 +- 17
|
0.19
|
0.14
|
0.21
|
0.05
0.91
|
|
VT
|
Intervention
Control
|
53 +- 23
52 +- 24
|
58 +- 23
68 +- 24
|
5 +- 20
6 +- 20
|
0.62
|
0.92
|
0.78
|
<0.01**
<0.01**
|
|
SF
|
Intervention
Control
|
77 +- 23
71 +- 26
|
83 +- 20
77 +- 25
|
6 +- 21
6 +- 20
|
0.03*
|
0.06
|
0.92
|
<0.01**
0.02*
|
|
RE
|
Intervention
Control
|
69 +- 41
55 + 43
|
73 +- 39
67 +- 41
|
5 +- 45
11 +- 43
|
<0.01**
|
0.15
|
0.34
|
0.15
0.02*
|
|
MH
|
Intervention
Control
|
74 +- 18
71 +- 19
|
78 +- 18
76 +- 19
|
3 +- 16
4 +- 17
|
0.24
|
0.39
|
0.77
|
<0.01**
0.03*
|
|
EQ-5D index
|
Intervention
Control
|
0.75 +- 0.20
0.73 +- 0.21
|
0.78 +- 0.20
0.75 +- 0.21
|
0.03 +- 0.23
0.00 +- 0.23
|
0.49
|
0.72
|
0.33
|
0.12
0.98
|
|
EQ-5D VAS
|
Intervention
Control
|
66 +- 23
62 +- 23
|
73 +- 18
73 +- 20
|
7 +- 22
11 +- 24
|
0.13
|
0.91
|
0.30
|
<0.01**
<0.01**
|
|
HADS-A
|
Intervention
Control
|
4.9 +- 4.0
5.0 +- 3.8
|
4.2 +- 3.7
4.4 +- 3.9
|
-0.7 +- 3.3
-1.0 +- 2.4
|
0.83
|
0.67
|
0.51
|
<0.01**
<0.01**
|
|
HADS-D
|
Intervention
Control
|
3.8 +- 3.4
4.1 +- 3.5
|
3.5 +- 3.2
4.0 +- 3.6
|
-0.1 +- 0.5
-0.1 +- 0.5
|
0.51
|
0.25
|
0.70
|
0.31
0.14
|
*p<0.05 **p<0.01 HRQoL, Health-related quality of life; SD, standard deviation; SF-36, Short form 36; PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health; EQ-5D, EuroQol 5 dimensions; VAS, visual analogue scale; HADS-A, Hospital anxiety and depression scale – anxiety score; HADS-D, Hospital anxiety and depression scale – depression
Health-related quality of life
At baseline, measured with the ASTA questionnaire, there were more patients in the control group who reported that they were unable to work (p=0.01), more who avoided spending time with acquaintances (p=0.03) and family/relatives (p=0.03). After one year the patients in the intervention group were to a higher degree free from a negative influence on HRQoL compared to patients in the control group, where more patients were unable to work (p = 0.01).
There were differences between the two groups at baseline also in SF-36 ([table 3]). Patients in the intervention group scored higher in four scales (PF, RP, SF and RE) compared to patients in the control group. After one year there was significant improvement in both groups in the scales RP, VT, SF, MH and additionally RE in the control group. Both patient groups improved in their scoring in EQ-VAS while there were no differences in the EQ-5D index. There were no significant differences between the groups at the one year follow-up ([table 3]).
Comparisons with the norm population
When comparing the two patient groups at baseline with a norm population assessed by SF-36, the patients in the intervention group scored significantly worse (p<0.05) in six out of eight scales (RP, GH, VT, SF, RE, MH) while the patients in the control group scored worse in seven of the scales (PF, RP, GH, VT, SF, RE, MH) ([figure 4]).
Figure 4. SF-36 scores (means) in the control and intervention groups at baseline and after one year compared to a Swedish norm population, aged 65 to 74 years.
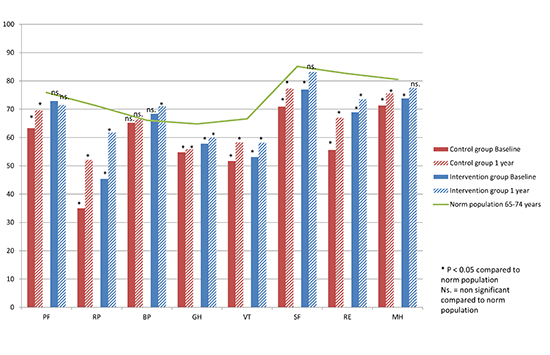
After one year, the patients in the intervention group improved in two scales (SF and MH) and scored similar to the norm population, and even better than the norm population in the scale BP. The patients in the control group still scored worse in seven out of eight scales, i.e. in all except BP, equal to the situation at baseline.
The main finding in this study on structured care given through an AF outpatient clinic was the significant improvement in guideline adherence. At the one-year follow-up the patients reached the HRQoL scores of a norm population to a higher degree compared to patients in the control group. Arrhythmia-specific symptoms were less frequently experienced in the intervention group and HRQoL improved, measured with the arrhythmia-specific questionnaire.
Several studies have shown a discrepancy between guidelines and everyday clinical practice in the management of AF[5], [16]. A Swedish study from 2002 showed that about 50 % of AF patients with indications for OAC actually received it[17]. Since the introduction of a risk factor-based approach for stroke prevention, i.e. CHADS2/CHA2DS2-VASc-scores, there has been a considerable improvement in guideline adherence concerning OAC treatment[16]. However, contemporary data still indicate significant both under- and over-treatment with OAC in patients with AF, which is associated with poorer outcome and emphasizes the importance of guideline implementation[16].
Although appropriate antithrombotic treatment was higher in the control group at follow-up than shown in the results from older studies[5] and consistent with new promising reports[16], the structured care resulted in a greater improvement in adequate use of OAC. Studies show that guideline adherence concerning AF management and especially antithrombotic treatment, is improving worldwide[16], but this study shows the importance of structured care in order to improve guideline adherence.
The structured care in this study resulted in improved guideline adherence. The results are consistent with a study conducted by Hendriks et al., which showed a significant improvement in guideline adherence leading to a significant reduction in cardiovascular mortality and hospitalisation[18]. Another similarity between these two studies is the patients’ reported measurements, where the patients in the control group had lower scores in symptom burden and HRQoL at baseline. In both studies, the scores of the generic SF-36 questionnaire improved in both groups, with no significant difference between the groups at follow-up[13]. Both studies suffer from a relatively large number of patients lost to follow-up, particularly regarding patients in the control group. However, in this study, the SF-36 scores were to a greater extent improved to the level of the norm population in the intervention group. Moreover, in the present study a disease-specific questionnaire was used, demonstrating differences in symptoms between the two groups. These differences remained after one year, in favour of the intervention group.
Furthermore, in the disease-specific instrument, the intervention group improved more in HRQoL than the control group. Using the ASTA questionnaire allows both detection and reflection of disease-specific changes between patients and over time. The well-known SF-36 and EQ-5D questionnaires, which are often used in AF studies, are generic and thereby reflect general health, which is influenced by comorbidities, commonly present in patients with AF. Recommendations urge the use of disease-specific instruments, especially when measuring changes in symptom burden and HRQoL over time[19].
The degree of anxiety was significantly reduced in both groups. The fact that anxiety is a strong predictor of HRQoL[6], [7] and that HRQoL can predict hospitalisation and mortality, emphasizes the importance of focusing on reducing anxiety in patients with AF. Treatment of patients with AF should thus focus on reducing symptoms, anxiety, depression and enhancing HRQoL in addition to being compliant with guidelines[19] .
Due to the complexity of the care of patients with AF, The Atrial Fibrillation Network and the European Heart Rhythm Association have recently highlighted the importance of development of structured patient-centred care, guided by risk profiling and symptom assessment. They also note that interdisciplinary dedicated AF services that incorporate lifestyle interventions are likely to facilitate such a structured model. They recommend the development of integrated and structured approaches to AF care led by interdisciplinary teams to improve the quality of care, and list the evaluation of structured care compared to current care as a research priority for the next five years[20]. Many of the recommendations mentioned above were carried out in this study, and the structured management was shown to improve the quality of care in patients with AF.
One important limitation is the non-randomised design of the study with the intervention group treated at one hospital while three other hospitals served as controls. This is probably the main reason for the observed differences at baseline. This design was probably also the reason for the relatively large number of patients not returning the questionnaires for follow-up, rendering the study underpowered to a certain extent.
Inclusion in the study was not consecutive for logistical reasons.
The study showed improvement in guideline adherence in the intervention group with structured AF care, mainly driven by improvement in OAC prescription. The degree of anxiety was reduced after one year and the scoring concerning HRQoL was improved in both patient groups. The arrhythmia-specific symptoms were less frequently experienced in the intervention group and HRQoL improved, and the SF-36 scores were more similar to the norm population compared to the control group at follow-up.