Active Implantable cardioverter-defibrillators in Continuous-flow Left Ventricular Assist Device Recipients
Kuldeep Shah1, Rahul Chaudhary2, Mohit K. Turagam3, Mahek Shah4, Brijesh Patel5, Gregg Lanier6, Dhanunjaya Lakkireddy7#, Jalaj Garg8#
1Division of Cardiology, Cardiac Arrhythmia Service, Beaumont Hospital, Oakland University William Beaumont School of Medicine, Royal Oak, Michigan.2Division of Cardiology, University of Pittsburgh Medical Center, Pittsburgh, PA.3Helmsley Electrophysiology Center, Icahn School of Medicine at Mount Sinai, New York, NY.4Division of Cardiology, Thomas Jefferson University Hospital, Philadelphia, PA.5Division of Cardiology, West Virginia University Medical Center, Morgantown, VW.6Division of Cardiology, Westchester Medical Center, New York Medical College, Valhalla, NY.7Cardiac Arrhythmia Service, Kansas City Heart Rhythm Institute and Research Foundation, Kansas City, KS.8Division of Cardiology, Cardiac Arrhythmia Service, Loma Linda University Health, Loma Linda, CA.#DL and JG are co-senior authors.
Implantable cardioverter-defibrillator (ICD) in patients with heart failure with reduced ejection fraction reduces mortality secondary to malignant arrhythmias. Whether end-stage heart failure (HF) with continuous-flow left ventricular assist device (cf-LVAD) derive similar benefits remains controversial.
We performed a systematic literature review and meta-analysis of all published studies that examined the association between active ICDs and survival in advanced HF patients with cfLVAD. We searched PubMed, Medline, Embase, Ovid, and Cochrane for studies reporting the association between ICD and all-cause mortality in advanced HF patients with cfLVAD. Mantel-Haenszel risk ratio (RR) random-effects model was used to summarize data.
Ten studies (9 retrospective and one prospective) with a total of 7,091 patients met inclusion criteria. There was no difference in all-cause mortality (RR 0.84, 95% CI 0.65–1.10, p=0.20, I2 =62.40%), likelihood of survival to transplant (RR 1.07, 95% CI 0.98–1.17, p= 0.13, I2 =0%), RV failure (RR 0.74, 95% CI 0.44–1.25, p = 0.26, I2 =34%) between Active ICD and inactive/no ICD groups, respectively. Additionally, 27.5% received appropriate ICD shocks, while 9.5% received inappropriate ICD shocks. No significant difference was observed in terms of any complications between the two groups.
All-cause mortality, the likelihood of survival to transplant, and worsening RV failure were not significantly different between active ICD and inactive/no ICD in cf-LVAD recipients. A substantial number of patients received appropriate ICD shocks suggesting a high-arrhythmia burden. The risks and benefits of ICDs must be carefully considered in patients with cf-LVAD.
Key Words : Implantable cardioverter-defibrillator, Continuous-flow LVAD, Mortality.
Jalaj
arg MD FACC FESC
Division of Cardiology, Cardiac Arrhythmia Service
Loma Linda University Health
11234 Anderson St, Loma Linda, CA 92354
Continuous flow left ventricular assist devices (cf-LVAD) are being increasingly utilized in patients with end-stage heart failure (on guideline-directed medical therapy) as a bridge to transplant or destination therapy, with improved overall survival 1,2. Similarly, implantable cardioverter-defibrillator (ICD) is indicated in heart failure patients (New York Heart Association functional class I, II, III) for primary/secondary prevention of sudden cardiac death caused by ventricular arrhythmias.
Patients with cf-LVAD are at increased risk of ventricular arrhythmias either due to worsening underlying disease substrate, scarring around the inflow cannula, or arrhythmias resulting from suction events due to underfilling of the left ventricle 3,4. However, it remains controversial if ICD offers any survival benefit in advanced heart failure patients with cf-LVAD. Patients with cf-LVAD have been able to tolerate prolonged periods of ventricular arrhythmias with minimal or no neurological sequelae, and are rarely associated with sudden cardiac death 5. Based on the currently available literature, there are no strict guidelines on ICD utilization in advanced heart failure patients with cf-LVAD. Therefore, we performed a systematic review and meta-analysis of all the clinical studies examining the role of active ICD in end-stage heart failure patients with cf-LVAD.
The reporting of this systematic review and meta-analysis complies with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines [] 6.
The initial search strategy was developed by two authors (KS and RC). Systematic search, without language restriction, using PubMed, EMBASE, SCOPUS, Google Scholar, and ClinicalTrials.gov from inception to November 10th, 2020, for studies comparing clinical outcomes between active ICD versus inactive ICD and/or no ICD in advanced heart failure patients with cf-LVAD was performed. We used the following keywords and medical subject heading: "continuous-flow left ventricular assist device," "implantable cardioverter-defibrillator," "end-stage heart failure."
Study Selection and data extraction
The eligibility criteria for our systematic review and meta-analysis included: (1) all studies reporting clinical outcomes comparing active ICD vs. inactive ICD/no ICD in end-stage heart failure patients with cf-LVAD and (2) studies that included human subjects aged ≥ 18 years. We included studies only published in the English language. Studies involving pulsatile flow LVAD (pf-LVAD), single-arm studies, case reports, editorial, or systematic reviews were excluded. Two investigators (KS and RC) independently performed the literature search and screened all titles and full-text versions of all relevant studies that met study inclusion criteria. The references of all identified articles were also reviewed for relevant studies meeting the eligibility criteria.
The data from included studies were extracted using a standardized protocol and a data extraction form. Any discrepancies between the two investigators were resolved with a consultation with the senior investigator (JG). Two independent reviewers (KS and RC) extracted the following data from the eligible studies: author name, study design, publication year, follow-up duration, number of patients, age, gender, body mass index, diabetes, smoking, etiology of cardiomyopathy, indications of cf-LVAD, medications, INTERMACS score. The Newcastle Ottawa Risk bias assessment tool was used to appraise the included studies' quality [].
The primary outcome of our study was - (1) All-cause mortality. Secondary outcomes were the likelihood of survival to transplant, right ventricular (RV) failure, and ICD therapies (appropriate or inappropriate). Adverse events included were infectious complications (sepsis or bacteremia or driveline infections), LVAD related complications (pump thrombosis or driveline malfunction or device malfunction), and neurological complications (hemorrhagic or ischemic).
Mantel-Haenszel risk ratio (RR) random-effects model (DerSimonian and Laird method) was used to summarize data between the two groups 7. For single arm proportion we used the Logit method to establish variance of raw proportions and then used random effects model (DerSimonian and Laird method) to combine the transformed proportions. The data of the pooled analysis was plotted on forest plots. Higgins I-squared (I2) statistic was used to assess the test of heterogeneity 8. A value of I2 of 0–25% represented insignificant heterogeneity, 26–50% represented low heterogeneity, 51–75% represented moderate heterogeneity, and more than 75% represented high heterogeneity. Publication bias was visually assessed using funnel plots and Egger's linear regression test of funnel plot asymmetry. A two-tailed p < 0.05 was considered statistically significant. Statistical analysis was performed using Comprehensive Meta-Analysis version 3.0 (Biostat Solutions, Inc. [BSSI], Frederick, Maryland).
A total of 329 citations were identified [Figure 1] during the initial search. Three hundred five records were excluded. After a detailed evaluation of these studies, ten studies (9 retrospective and one prospective) ultimately met the inclusion criteria (N=7,091 patients) 9-18. The follow-up duration for the studies ranged from 52 days to 3.1 years. [Table 1] summarizes the study characteristics of the included trials.
Figure 1. Flow Diagram illustrating the systematic search of studies
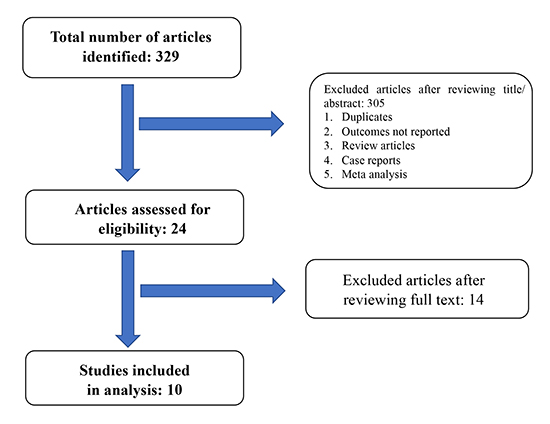
Table 1. Baseline characteristics of studies included in our meta-analysis.
| Study |
Anderson et al |
Enriquez et al |
Garan et al |
Lee et al |
Clerkin et al. INTERMACS |
Clerkin et al. UNOS |
Kutyifa et al |
Alvarez et al |
Cikes et al |
Simsek et al |
| Design |
Retrospective |
Retrospective |
Prospective |
Retrospective |
Retrospective |
Retrospective |
Retrospective |
Retrospective |
Retrospective |
Retrospective |
| Study period |
2006-2008 |
2008-2012 |
2012 |
2004-2013 |
2006-2016 |
2004-2014 |
2008-2014 |
2004-2017 |
2006-2018 |
2010-2016 |
| Sample size |
ICD: 17
No ICD: 6 |
ICD: 62
No ICD: 36 |
ICD: 77
No ICD: 17 |
ICD: 63
No ICD: 31 |
ICD: 2209
No ICD: 2209 |
ICD: 506
No ICD: 506 |
ICD: 129
No ICD: 62
Of 62, 31 had ICD implanted after cf-LVAD
|
ICD: 387
No ICD: 99
Of 99, 52 had ICD after cf-LVAD
|
ICD: 240
No ICD: 208
|
ICD: 104
No ICD: 123
|
| Follow up |
ICD: 214 days
No ICD: 52 days
|
253 ± 194 days |
12.7 ± 12.3 months |
364 ± 295 days |
12.4 months (median) |
ICD: 287.5 days (median)
No ICD: 305 Days (median)
|
2.1 ± 1 years |
401 days (median) |
1.1 years (median) |
16.5 ± 11.8 months |
| Patient age
mean ± SD (years) |
- |
ICD: 56.7
No ICD: 56.3
|
ICD: 63.1
No ICD: 58.1
|
ICD: 53.9
No ICD: 42.9
|
ICD: 59
No ICD: 59
|
ICD: 51
No ICD: 52
|
ICD: 57.4
No ICD: 54.9
|
ICD: 57
No ICD: 48.4
|
ICD: 54±12
No ICD: 50±14
|
ICD: 51.3 ± 12.2
No ICD: 49.3± 13.9
|
| Bridge to transplant |
19 total |
ICD: 55
No ICD: 33 |
ICD: 37
No ICD: 9
|
ICD: 56
No ICD: 28
|
ICD: 512
No ICD: 512
|
ICD: 506
No ICD: 506
|
ICD: 98
No ICD: 23
|
ICD: 257
No ICD: 24
|
ICD: 168
No ICD: 137
|
ICD: 91
No ICD: 103
|
| Device type |
HeartMate II |
HeartMate II |
- |
Ventrassist,Heartware |
- |
HeartMate II, Heartware |
HeartMate II |
- |
HeartMate II
HeartWare
HVAD
HeartMate3
|
Heartmate II, HeartMate III, HeartWare, HeartAssist5 |
| Diabetes |
- |
- |
- |
ICD: 17.46%
No ICD: 12.90 %
|
ICD: 4.5 %
No ICD: 4.2%
|
ICD: 27.9%
No ICD: 29.1%
|
ICD: 43%
No ICD: 29%
|
ICD: 158
No ICD: 29
|
ICD: 22.1%
No ICD: 17.8%
|
ICD: 26.9 %
No ICD: 29.3 %
|
| Body mass index |
- |
- |
- |
- |
ICD: 27.7
No ICD: 27.8
|
ICD: 27.5
No ICD: 27.4
|
ICD: 29.8
No ICD: 29.9
|
ICD: 28.5
No ICD: 27.2
|
ICD: 26.2 ± 4.8
No ICD: 25.3 ± 4.4
|
- |
| INTERMACS profile ≤ 2
|
- |
ICD: 45.2%
No ICD: 66.7%
|
ICD: 67.5%
No ICD: 88.2%
|
ICD: 73%
No ICD: 74.19%
|
ICD: 59.7 %
No ICD: 57.8%
|
- |
ICD: 52.7%
No ICD: 79%
|
ICD: 12.1%
No ICD:
49.49%
|
ICD:31.6%
No ICD:
56.7%
|
ICD: 27.9 %
No ICD:
36.6 %
|
| Ischemic cardiomyopathy |
- |
ICD: 30.7%
No ICD: 58.3%
|
ICD: 50.6%
No ICD: 58.8%
|
ICD: 31.74%
No ICD: 35.48%
|
ICD: 50.7%
No ICD: 48.6 %
|
ICD: 42.5%
No ICD: 42.1%
|
ICD: 47%
No ICD: 74.19%
|
ICD: 39.8%
No ICD: 48.48%
|
ICD: 42.5%
No ICD: 50%
|
ICD: 46.2%
No ICD: 52.8 %
|
| Medications
Beta-
blockers |
- |
- |
ICD: 96.1%
No ICD: 52.9% |
ICD: 71.4%
No ICD: 67.74%
|
ICD: 70.1%
No ICD: 72.3%
|
- |
ICD: 84%
No ICD: 56.45 %
|
- |
ICD: 78.3%
No ICD: 43.5%
|
ICD: 73.1%
No ICD:
71.5 %
|
| ACE Inhibitors/ARB |
|
|
- |
ICD: 65.07%
No ICD: 67.74%
|
- |
|
ICD: 30%
No ICD: 22.58 %
|
|
ICD: 49.3%
No ICD: 49.7%
|
ICD: 31.7%
No ICD: 33.3 %
|
| Antiarrhythmic medications |
|
|
ICD: 37.7%
No ICD: 52.9 %
|
ICD: 41.26%
No ICD: 38.70%
|
ICD: 40.4%
No ICD: 41.4%
|
|
- |
|
- |
ICD: 25 %
No ICD:12.2%
|
The study by Cantillon et al. evaluated outcomes of ICD in both pf-LVAD (n = 354) and cf-LVAD patients; however, the baseline characteristics and outcomes of patients with cf-LVAD could not be delineated from those who underwent pf-LVAD. Hence, we excluded from our analysis 19. In studies by Kutyfia et al., Alvarez et al., and Cikes et al., a total of 103 patients received ICD post-cf-LVAD implantation; and were therefore included in the ICD group 15-17. In a study by Cikes et al., 20 patients received ICD post-cf-LVAD, while 45 patients had their ICD deactivated or extracted post-cf-LVAD implantation, 34 of which underwent heart transplantation 17. Studies by Clerkin et al. (INTERMACS and UNOS data) were propensity score-matched in order to ensure comparable groups (and similar baseline characteristics). This accounted for more than two-thirds (76.5%) of our study population (n=5,430) 13,14.
Overall, the patients' mean age was 50.34 years in active ICD and 47.09 years in the inactive/no ICD group. Bridge to transplantation was the indication for LVAD placement in 3,174 patients (44.70%). [Table 1] summarizes the study characteristics of the included trials.
The data for all-cause mortality was available in all ten trials 9-18. Active ICD was not associated with any difference in all-cause mortality as compared to Inactive/No ICD (RR 0.84, 95% 0.65-1.10, p = 0.20). Moderate heterogeneity was observed between trials (I2 =62.40%). Publication bias was observed [Figure 3].
Figure 2. Active ICD versus inactive ICD/no ICD in end-stage heart failure patients with cf-LVAD.
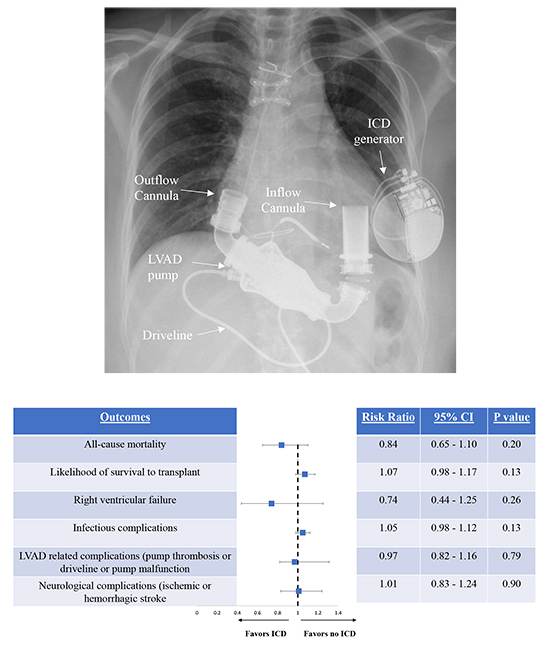
Figure 3. All-cause mortality.
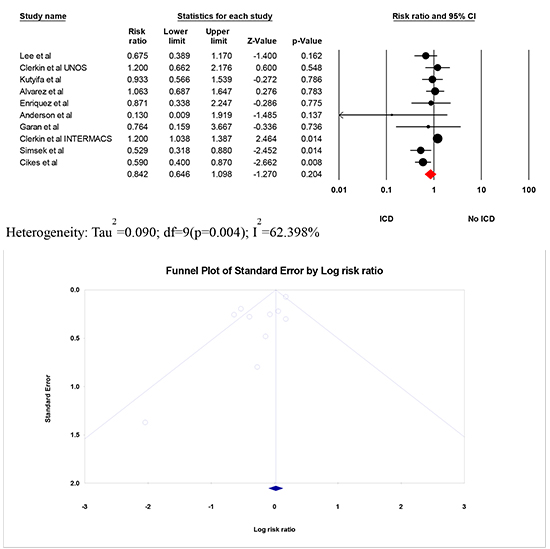
The Forest plot shows the outcomes of the individual trials as well as the aggregate. Point estimates to the left favor active ICD. The funnel plot demonstrates publication bias.
Likelihood of Survival to Transplant
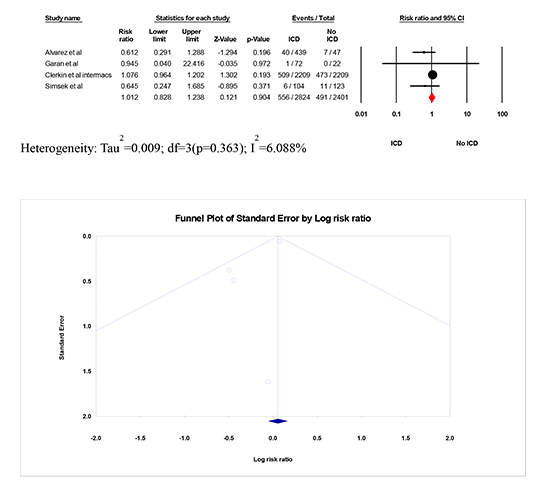
The data for the likelihood of heart transplant was available in six trials 10-14,18. No significant difference was observed between the two groups in the likelihood of survival to transplant (RR 1.07, 95% CI 0.98 – 1.17, p = 0.13). No significant heterogeneity was observed between trials (I2 =0%). No publication bias was observed [Figure 4].
Figure 4. Likelihood of Survival to Transplant.
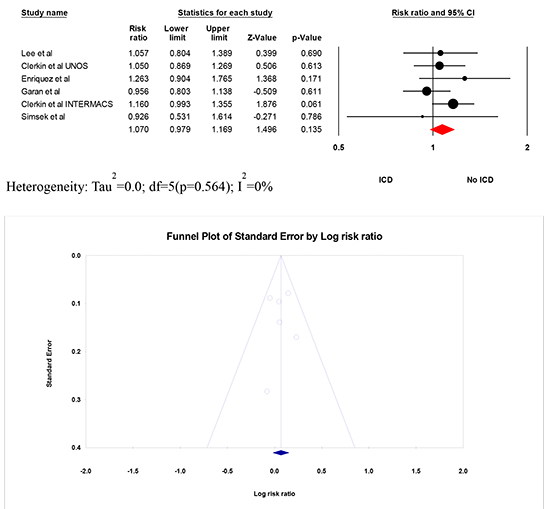
The Forest plot shows the outcomes of the individual trials as well as the aggregate. Point estimates to the left favor active ICD. The funnel plot demonstrates no publication bias.
Right ventricular failure
The data for right ventricular (RV) failure was available in five trials 10-12,16,18. No significant difference was observed in terms of RV failure between the two groups (RR 0.74, 95% CI 0.44 – 1.25, p = 0.26). Mild heterogeneity was observed between trials (I2 =34.44%). No publication bias was observed [Figure 5].
Figure 5. Right ventricular failure.
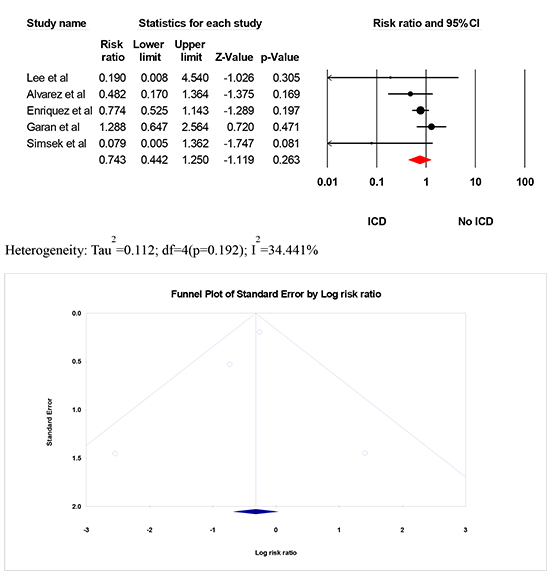
The Forest plot shows the outcomes of the individual trials as well as the aggregate. Point estimates to the left favor active ICD. The funnel plot demonstrates no publication bias.
We conducted a separate literature search in PUBMED, MEDLINE, EMBASE, EBSCO, CINAHL, Web of Science, and Cochrane (March 10th, 2020) to identify eligible studies assessing ICD shocks (both appropriate and inappropriate) in end-stage heart failure patients with cf-LVAD. After a detailed evaluation of these studies, eight studies (7 retrospective and one prospective) clinical studies ultimately met the inclusion criteria (N=970 patients). Follow-up duration for the studies ranged from 52 days to 3 years. [Table 2] summarizes the study characteristics of the included trials 9,10,12,15-17,20,21. Studies by Oswald et al. 21 and Brenyo et al. 20 were only included to assess the incidence of ICD shocks (since both studies did not have any comparator arm).
Table 2. Baseline characteristics of studies included in our meta-analysis evaluating ICD shocks (appropriate or inappropriate)
| Study ID |
Anderson et al |
Lee et al |
Enriquez et al |
Kutyifa et al |
Alvarez et al |
Cikes et al |
Oswald et al |
Brenyo et al |
| Design |
Retrospective |
Retrospective |
Retrospective |
Retrospective |
Retrospective |
Retrospective |
Prospective |
Retrospective |
| Study period |
2006-2008 |
2004-2013 |
2008-2012 |
2008-2014 |
2004-2017 |
2006-2018 |
2005-2008 |
2006-2010 |
| Sample size |
ICD: 17
No ICD: 6
|
ICD: 63
No ICD: 31
|
ICD: 62
No ICD: 36
|
ICD: 129
No ICD: 62
Of 62, 31 had ICD after cf-LVAD
|
ICD: 387
No ICD: 99
Of 99, 52 had ICD after cf-LVAD
|
ICD: 240
No ICD: 208
|
ICD only: 61 |
ICD only: 61 |
| Follow up |
ICD: 214 days
No ICD: 52 days
|
364 ± 295 days |
253 ± 194 days |
2.1 ± 1 years |
401 days (median) |
1.1 years (median) |
365 + 321 days. |
622 days |
| Patient age
mean ± SD (years)
|
- |
ICD: 53.9
No ICD: 42.9
|
ICD: 56.7
No ICD: 56.3
|
ICD: 57.4
No ICD: 54.9
|
ICD: 57
No ICD: 48.4
|
ICD: 54±12
No ICD: 50±14
|
ICD only: 50+12 |
ICD only: 55.75 |
| Bridge to transplant |
19 total |
ICD: 56
No ICD: 28
|
ICD: 55
No ICD: 33
|
ICD: 53
No ICD: 17
|
ICD: 226
No ICD: 55
|
ICD: 73%
No ICD: 68.8%
|
- |
ICD only: 72% |
| Device type |
HeartMate II |
Ventrassist, Heartware
|
HeartMate II |
HeartMate II |
- |
HeartMate II
HeartWare
HVAD
HeartMate 3
|
HeartMate II
HeartWare
|
HeartMate II
Jarvik
|
| Diabetes |
- |
ICD: 17.46%
No ICD: 12.90 %
|
- |
ICD: 43%
No ICD: 29%
|
ICD: 158
No ICD: 29
|
ICD: 22.1%
No ICD: 17.8%
|
- |
ICD only: 361% |
| Body mass index |
- |
- |
- |
ICD: 29.8
No ICD: 29.9
|
ICD: 28.5
No ICD: 27.2
|
ICD: 26.2 ± 4.8
No ICD: 25.3 ± 4.4
|
- |
- |
| INTERMACS profile ≤ 2
|
- |
ICD: 73%
No ICD: 74.19%
|
ICD: 45.2%
No ICD: 66.7%
|
ICD: 52.7%
No ICD: 79%
|
ICD: 12.1%
No ICD: 49.49%
|
ICD:31.6%
No ICD: 56.7%
|
- |
- |
| Ischemic cardiomyopathy |
- |
ICD: 31.74 %
No ICD: 35.48%
|
ICD: 30.7%
No ICD: 58.3%
|
ICD: 47%
No ICD: 74.19%
|
ICD: 39.8%
No ICD: 48.48%
|
ICD: 42.5%
No ICD: 50%
|
ICD only: 49% |
ICD only: 60.6% |
| Medications Beta- blockers
ACE Inhibitors/ARB
Antiarrhythmic medications |
|
ICD: 71.4%
No ICD: 67.74%
ICD: 65.07%
No ICD: 67.74%
ICD: 41.26%
No ICD:
38.70%
|
- |
ICD: 84%
No ICD:
56.45 %
ICD: 30%
No ICD: 22.58 %
-
|
- |
ICD: 78.3%
No ICD: 43.5%
ICD: 49.3%
No ICD: 49.7%
-
|
ICD only: 69%
ICD only: 67%
ICD only: 71%
|
ICD only: 90%
ICD only: 63.9%
ICD only: 32.78%
|
The data for appropriate ICD shock was available in all eight trials 9,10,12,15-17,20,21 that included 970 patients, with an incidence of 27.5% (95% CI 0.22-0.33, I2=61.36%) during the follow-up period [Figure 6].
Figure 6. Forest Plot of the Incidence of Appropriate ICD shock in patients with cf-LVAD.
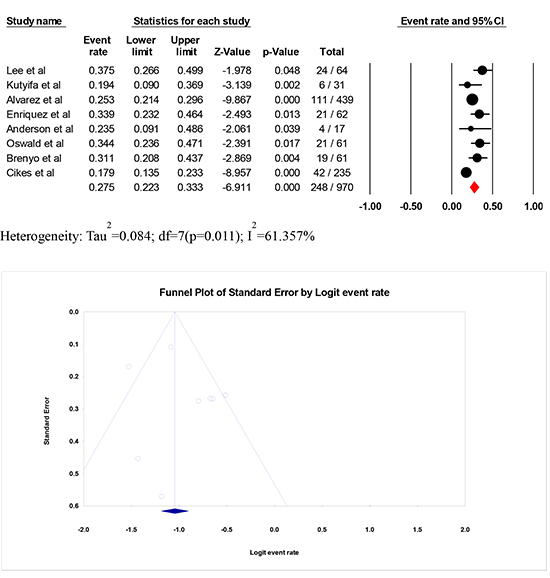
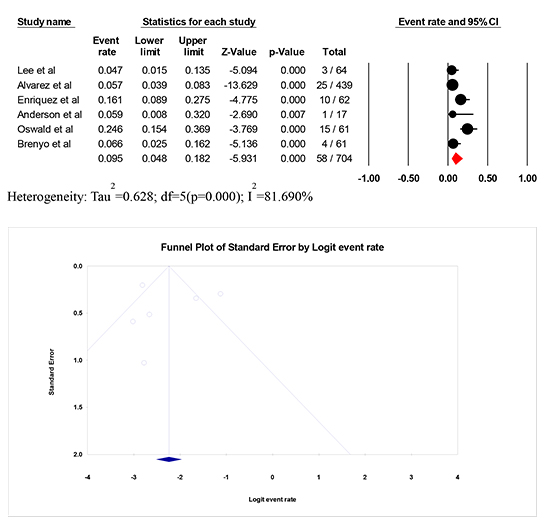
Inappropriate ICD shock was reported in six trials 9,10,12,16,20,21 that included 704 patients with an incidence rate of 9.5% (95% CI 0.05-0.18, I2=81.69%) during the follow up period [Figure 7].
Figure 7. Forest Plot of the Incidence of Inappropriate ICD shock in patients with cf-LVAD.
The major adverse event rates were reported in six clinical trials [Table 3]. There was no significant difference in terms of infectious complications (RR 1.05, 95% CI 0.98-1.12, p = 0.13, I2=0%) [Figure 8] 11-13,16-18, LVAD related complication (19.72% vs 21.94%; RR 0.97, 95% CI 0.82-1.16, p=0.79, I2=19.76%) [Figure 9] 10,13,16,18 and neurological complications (ischemic or hemorrhagic stroke) (19.68% vs 20.44%; RR 1.01, 95% CI 0.83-1.24, p=0.90, I2=6.1%) [Figure 10] 11,13,16,18 between the two groups. The test of heterogeneity was not significant for either outcomes. No publication bias was observed.
Figure 8. Infectious complications (sepsis or bacteremia or driveline infection).

The Forest plot shows the outcomes of the individual trials as well as the aggregate. Point estimates to the left favor active ICD. The funnel plot demonstrates no publication bias.
Figure 9. LVAD related complications (pump thrombosis or driveline malfunction, or device malfunction).
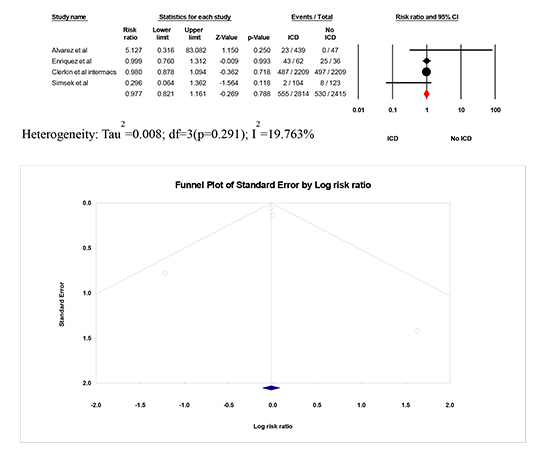
The Forest plot shows the outcomes of the individual trials as well as the aggregate. Point estimates to the left favor active ICD. The funnel plot demonstrates no publication bias.
Figure 10. Neurological complications (ischemic or hemorrhagic stroke).
The Forest plot shows the outcomes of the individual trials as well as the aggregate. Point estimates to the left favor active ICD. The funnel plot demonstrates no publication bias.
Table 3. Adverse events reported in studies included in our meta-analysis
|
Garan et al |
Enriquez et al |
Lee et al |
Clerkin et al. INTERMACS |
Alvarez et al |
Simsek et al |
Cikes et al |
|
ICD (72) |
No ICD (22) |
ICD (62) |
No ICD (36) |
ICD (64) |
No ICD (36) |
ICD (2209) |
No ICD (2209) |
ICD (439) |
No ICD (47) |
ICD (104) |
No ICD (123) |
ICD |
No ICD |
| Infection |
1 |
1 |
NR |
NR |
0 |
4 |
1046 |
992 |
110 |
9 |
5 |
11 |
risk ratio
(separate events not reported) |
| LVAD complications |
NR |
NR |
43 |
25 |
NR |
NR |
487 |
497 |
23
Pump thrombosis: 20
Driveline malfunction: 2
Device malfunction: 1
|
0 |
2
Pump thrombosis: 2
|
8
Pump thrombosis: 8
|
NR |
NR |
| Neurological complications |
1 |
0 |
NR |
NR |
NR |
NR |
509 |
473 |
4 |
7 |
6 |
11 |
NR |
NR |
N.R = not reported, ICD = Implantable cardioverter defibrillator
A sensitivity analysis was performed to investigate the significant heterogeneity observed between the trials for all-cause mortality. Studies by Clerkin et al. (INTERMACS and UNOS data) 13,14 were propensity score-matched in order to ensure comparable groups (and similar baseline characteristics). This accounted for more than two-thirds (76.5%) of our study population (n=5,430), of which Clerkin eta l (INTERMACS) contributed 81.36% patients (n=4,418). While Clerkin et al. (UNOS) included all patients as bridge to transplant, only 23.17% of patients were as bridge to transplant in the Clerkin et al. (INTERMACS) trial. There was a significant reduction in all-cause mortality in cf-LVAD recipients with active ICD (RR 0.77, 95% CI 0.61-0.98, p = 0.03), with no significant heterogeneity (P for heterogeneity = 0.22, I2 = 24.86%) after excluding Clerkin et al (INTERMACS) trial.
Finally, we performed a sensitivity analysis after excluding both Clerkin et al. trials (UNOS and INTERMACS). There remained a significant reduction in all-cause mortality in cf-LVAD with active ICD (RR 0.73, 95% CI 0.58 – 0.92, p = 0.01, I2 = 15.12%, P for heterogeneity = 0.31).
The main findings in this analysis are: (1) All-cause mortality and likelihood of survival to transplant did not differ between the Active ICD and Inactive/no ICD groups in end-stage heart failure patients with cf-LVAD; (2) the incidence rate of appropriate ICD shock was 27.5%, while inappropriate ICD shock was 9.5%; (3) no significant increase in the incidence of RV failure; and finally, there was no difference in the adverse events between the two groups. These findings have important clinical implications, and therefore, the risks and benefits of active ICD must be carefully considered [Figure 2].
This is the largest study assessing the role of active ICD in end-stage heart patients with cf-LVAD (either as destination therapy or bridge to transplant). Our findings strengthen the results of the previously reported trials and metanalyses, demonstrating no net clinical benefit of ICD in advanced heart failure patients with cf-LVAD 22,23. Since then, new clinical trials and more contemporary data mandated an update to the prior meta-analyses. There are several potential explanations for the findings observed in our study. First, given the lack of randomized clinical trials (and exclusion of healthier patient population), no mortality benefit with ICD is a mere reflective of selection bias towards sicker patient population. Second, end-stage heart failure patients with cf-LVAD are at increased risk of death from non-arrhythmic causes such as pump failure, infections, or device thrombosis, thus making it difficult to assess the net clinical benefit of ICD's. Third, patients with cf-LVAD may be less susceptible to unfavorable effects of ventricular arrhythmia (as noted in our study) 5,24; consequently, are less likely to derive mortality benefit from ICD. Lastly, with improved cf-LVAD technology, patient management, and care transition teams, might have led to improved survival that counteracted the effect of ICD. This explains why there was no mortality benefit observed in our study in comparison to previously published meta-analysis assessing the role of ICD in advanced heart failure and pulsatile LVAD22 (although results should be interpreted with caution given significant heterogeneity observed in our analysis).
The role of ICD in patients with cf-LVAD remains unclear, with no clear consensus from the American College of Cardiology/American Heart Association. The International Society of Heart and Lung Transplantation guidelines recommends the use of ICD [either reactivating previously implanted ICD (Class I, level of evidence A) or de novo implantation of ICD after cf-LVAD (Class IIa, level of evidence B)] 25. This recommendation is solely based upon a single retrospective study in advanced heart failure patients with pulsatile LVAD26. Studies have shown pre-LVAD ventricular arrhythmia is a significant predictor of ventricular arrhythmias post-implant, with increased risk within the first 30 days following LVAD implant 27. Mechanistically, pulsatile LVAD relies partially on intrinsic pump function, sustained and prolonged ventricular arrhythmias might, therefore, result in pump failure, hemodynamic decompensation, and unfavorable prognosis. On the contrary, cf-LVAD may permit preserved pump function and prevent hemodynamic decompensation during sustained ventricular arrhythmias. However, severe RV failure (due to unsupported RV) may result in adverse clinical outcomes (worst survival and increased heart failure hospitalizations) in 10-40% LVAD patients 28. Therefore, termination of ventricular arrhythmias in cf-LVAD patients with unsupported RV might be a reasonable option. Besides, patients with cf-LVAD are also at increased risk of ventricular arrhythmias (from increased arrhythmogenic milieu from suction events) compared to pulsatile flow LVAD; therefore, having active ICD in situ seems logical. Furthermore, with a 27.5% incidence of appropriate ICD shocks (in contrast to 9.5% inappropriate ICD shocks), it appears more reasonable to activate ICD therapies following cf-LVAD implantation. Given increasing evidence of the decreased quality of life and increased mortality with ICD shocks, we, therefore, recommend delayed therapy approach (i.e., either prolonged detection time or higher rate cut-offs) in patients with cf-LVAD ([Table 4] highlights proposed programming setting across different device vendors). We also recommend setting a lower VT monitor zone, and closer follow-up (either in electrophysiology clinic or remote monitoring) to look for arrhythmic burden.
Table 4. Proposed programming setting across different device vendors in patients with cf-LVAD and ICD
|
Biotronik |
Boston Scientific |
Medtronic |
St. Jude Medical |
| VT detection |
190 bpm
80 intervals to detect
20 intervals to redetect
|
190 bpm
60 seconds to detect
|
188 bpm
100 intervals to detect (33 seconds)
52 intervals to redetect
|
190 bpm
100 intervals to detect (33 seconds)
6 intervals to redetect
|
| VF detection |
250 bpm
30/40 intervals
12/16 intervals to redetect
|
≥ 250 bpm
15 seconds to detect
|
250 bpm
30/40 intervals
12/16 intervals to redetect
120/160 beats to detect (32.4 seconds)
30/40 beats to redetect
|
≥ 250 bpm
100 intervals to detect (25 seconds)
6 intervals to redetect
|
In our study, no significant difference was observed in terms of infectious complications in cf-LVAD patients between the two groups. ICD related infections may disseminate locally (to cannula and pump) and systemically, requiring long-term suppressive antibiotics, and/or urgent heart transplant or LVAD exchange, which is associated with approximately 30% one-year mortality, and increased health care cost and burden. Despite no significant difference in the adverse effects between the two groups, it still remains unclear at this time if there is an added advantage of de novo implantation of ICD after cf-LVAD. However, it seems reasonable to pursue generator exchange in secondary prevention patients or those with any pacing indications (although our study was not designed to assess this outcome in particular).
Our study has several important limitations. First, patient selection bias due to the retrospective nature of the included studies could not be excluded. Second, the decision and timing for ICD implantation/ICD programming parameters in cf-LVAD patients were not well defined. Third, information on arrhythmia burden/morphology and its timing in relation to LVAD implantation were inaccessible. Forth, patient-level data or right heart catheterization hemodynamics or arrhythmia details/ICD therapies stratified by LVAD type were not available. Fifth, the etiology of death (cardiac, or non-cardiac) could not be ascertained in all trials. Our meta-analysis results were primarily driven by the two largest included studies (UNOS and INTERMACS), accounting together for more than two-thirds of the total study population.
All-cause mortality, the likelihood of survival to transplant, and worsening RV failure were not significantly different between active ICD and inactive/no ICD in cf-LVAD recipients. However, there was an increased burden of ventricular arrhythmias in our pooled analysis, as evident by a 27.5% appropriate ICD shock rate, suggesting active ICD might be a practical decision in selected patients with cf-LVAD. Future research should be directed to study the safety and efficacy of active ICD's in end-stage heart failure patients with cLVAD in a dedicated randomized controlled study.