Long Term Outcome and Pulmonary Vein Reconnection of Patients Undergoing Cryoablation and/or Radiofrequency Ablation: Results from The Cryo Versus RF Trial.
Ang R, Hunter RJ, Lim WY, Opel A, Ullah W, Providencia R, Baker V, Finlay MC, Dhinoja MB, Earley MJ, Schilling RJ*
*
Barts Heart Centre, St Bartholomew’s Hospital, Barts Health NHS Trust, London, UK..
Long term prospective data comparing the efficacy of radiofrequency (RF) and cryoballoon ablation (CRYO) for paroxysmal atrial fibrillation (PAF) is lacking. We report the long-term outcomes of a randomized control trial comparing CRYO to RF ablation, or a novel COMBINED approach (RF followed by CRYO) for PAF. We studied the number and pattern of pulmonary vein (PV) reconnections in patients undergoing repeat procedure(s). The COMBINED approach had significantly higher single procedure success rate and is associated with the fewest reconnected PVs.
203 patients who underwent first time PAF ablation in a randomized clinical trial comparing CRYO (67), RF (67) and COMBINED (69) approaches were followed up. All patients with symptomatic recurrence of AF were offered a repeat procedure(s). Reconnected PV(s) at repeat procedure(s) were recorded. In a subset, the PV reconnection sites during the first repeat procedure were prospectively assessed and categorised into one of 8 segments. .
At 5 years, 57% of COMBINED patients remained free of AF after a single procedure compared to 47% CRYO and 19% RF patients (p<0.001 COMBINED vs RF and CRYO vs RF, p=0.043 COMBINED vs CRYO). During the first repeat procedure, theCOMBINED group had less number of reconnected PVs (mean number of reconnected PVs in the COMBINED group 1.2 vs 2.3 CRYO and 2.4 RF, p=0.034). There was a different pattern of PV reconnection comparing the CRYO and RF groups.
The COMBINED approach had a significantly higher single procedure success rate with fewer reconnected PVs and fewer reconnection sites compared to either CRYO or RF alone. CRYO in turn was superior to RF. PV reconnection pattern differed between CRYO and RF and the synergistic effect of the COMBINED approach may explain the improved single procedure efficacy.
Key Words : Atrial Fibrillation, Catheter Ablation, Radio frequency Catheter Ablation, Cryo Balloon Ablation, Pulmonary Vein Reconnection, Long Term Outcomes.
Correspondence to: Schilling RJ,
Barts Heart Centre, Barts Health NHS Trust,
London,UK
Catheter ablation to isolate pulmonary veins (PVs) is an effective treatment for drug-refractory paroxysmal atrial fibrillation (PAF) [1,2]. PV isolation is conventionally achieved using radiofrequency (RF) energy to create contiguous and transmural point-to-point lesions encircling the veins [1]. This is however time consuming, technically challenging and PV reconnection causing AF recurrence remains a problem [2,3].
A balloon-based approach using cryothermal energy has emerged as a comparable alternative with the potential of isolating PVs with a ‘single-shot’ technique and associated with lower risk of thermal injury and PV stenosis compared to radiofrequency (RF) energy sources [4]. A recent systematic review has suggested good acute procedural safety and efficacy with a one year freedom from AF of 73% [5]. Our own randomised control trial (The Cryo Versus RF Trial) comparing segmental ostial isolation with cryoballoon to wide antral circumferential ablation (WACA) of PVs using RF energy and a novel approach combining both found that cryoballoon and the combined approach were both superior to the conventional RF approach at 1 year. There was no significant difference between using cryoballoon alone compared to the combined approach [6].
However, long term prospective data comparing the efficacy of cryoballoon and RF ablation is lacking. Furthermore, there are little data comparing ablation strategies with respect to the extent and pattern of PV reconnection. In this study, we sought to address this by following up the cohort of patient in The Cryo Versus RF trial, looking at the long-term outcome following ablation and studying the distribution and pattern of PV reconnection during the repeat procedure.
234 patients undergoing first-time catheter ablation of PAF were randomized to cryoballoon (CRYO, n=78), radiofrequency (RF, n=77), or a novel cryoballoon and radiofrequency combined procedure (COMBINED, n=79) at a single institution as part of a randomized controlled trial (The Cryo Vs RFA trial), the results of which have been reported [6]. The study was approved by the local research ethics committee and was prospectively registered on NIH clinicaltrials.gov (NCT01038115). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Briefly, patients enrolled were aged over 18 years, had documented paroxysmal AF on at least two occasions and accepted for catheter ablation for AF. Patients were excluded from the trial if they had severe left atrial dilatation (greater than 50mm in diameter), severe valvular disease, or previous left atrial ablation.
Catheter ablation procedures
All patients underwent trans-oesophageal echocardiography pre-procedure and were anticoagulated without interruption. The procedures were performed under local anaesthetic (lidocaine), and conscious sedation (midazolam and diamorphine). A quadripolar catheter was inserted into the coronary sinus and a multipolar circular mapping catheter was used for mapping of the PVs. Double transseptal puncture was performed when dual transseptal access was required.
For CRYO, a 28mm and/or a 23mm first generation Arctic Front cryoballoons (Medtronic, Minneapolis, MN, USA) used. Retrograde PV angiography was used to demonstrate occlusion. Two freezes of up to 300s were performed initially in each PV with phrenic nerve pacing for the right-sided treatments. Further freezes were delivered if the veins were not isolated. If this approach failed, the operator could take the alternative cryoballoon size or complete PV isolation using focal ablation. Focal lesions were applied with an 8 mm cryoablation catheter (Freezor Max, Medtronic,Minneapolis, MN,USA), and if this failed a 3.5 mm RF ablation catheter (Thermocool Celsius, Biosense Webster, Diamond Bar, CA, USA) was used.
For RF, ablation energy was delivered using an irrigated F curve 3.5 mm non-contact force sensing ablation catheter (Navistar Thermocool, Biosense Webster, Diamond Bar, CA, USA) guided using CARTO 3 (Biosense Webster, Diamond Bar, CA, USA). Patients underwent WACA, with lesions placed 1–2 cm outside the PV ostia to isolate them in ipsilateral pairs. Power was limited to 30W and flow was adjusted from 2 mL/min up to 30 mL/min to achieve this without exceeding temperature limit of 480C.
For COMBINED, patients initially underwent WACA as in the RF group, with electrical isolation demonstrated using the circular mapping catheter followed by two further 5 min freezes using the cryoballoon, judged by good PV occlusion on venogram and temperatures of ≤ -400C.
In all cases, electrical isolation of all PVs was the end point for the procedures.
All antiarrhythmic drugs were stopped post procedure and patients were followed up at 3, 6 and 12 months with a 7 day Holter recording. There was open access to arrhythmia nurse specialists subsequently and further ambulatory monitoring prompted by symptoms. All patients with recurrence of symptoms and documented atrial arrhythmias lasting greater than 30s after the blanking period of 3 months were offered a repeat procedure. Attempts were made to contact all the patients for review between 1 April to 31 May 2017 to determine any adverse events, recurrences of AF/AT, current medications and symptoms. Patients with follow-up of less than 18 months were excluded from analysis.
Success was defined as freedom from documented AF/AT lasting at least 30 seconds following a 3-month blanking period. The primary endpoint of the study was the success rate following a single procedure without antiarrhythmic drugs. Secondary endpoint was the success rate at last follow-up after one or more procedures off and on antiarrhythmic drugs.
PV reconnection sites at first repeat procedure
All repeat procedures were performed with RF ablation using an open irrigated-tip catheter in conjunction with an electroanatomic mapping system. Using the multipolar circular mapping catheter, PV potentials were sequentially mapped and ablated until PV isolation. The positions of all reconnected PVs were prospectively documented.
In a subset of patients during the first repeat procedure, the PV reconnection sites of each individual PV were prospectively documented. Each PV was categorized into eight individual segments as described by Valles et al [7]and was used to describe PV reconnection patterns. The site of the earliest PV potential was mapped and categorized into one of the eight segments. If antral ablation at that site eliminated all PV potentials, the respective PV was found to have a single conduction gap. If ablation resulted in a change in activation sequence, the earliest PV potential was mapped and ablated until complete PVI was achieved. Hence, more than one reconnection sites were possible per PV.
Continuous data are presented as mean ± standard deviation if normally distributed or median ± inter quartile range if not. Categorical data are described as count (percentage). Continuous data were compared using Student’s t-test. Categorical data were compared using a chi-squared test and further pair-wise comparisons used Fisher’s exact test. Differences in survival on the Kaplan Meir curve was compared by log rank test. Univariate analysis was performed to assess for differences between groups and association of clinical characteristics with AF/AT recurrence. In all instances, a P value of <0.05 was considered statistically significant. Analysis was performed using SPSS version 24 (IBM, NY, USA) and Prism 6 (GraphPad, CA, USA).
Of the 234 patients in the original study, 203 patients (67 RF, 67 CRYO and 69 COMBINED) had follow-up of at least 18 months and were included in this analysis. The median follow-up duration was 5 years (IQR 3.6 to 6.4 years). [Table 1] compares the patient characteristics between the treatment groups, stratified by AF recurrence following a single procedure. There were no significant differences between the groups and no predictors of recurrence on univariate analysis.
Table 1. Patient characteristics.
|
RF (n=67) |
|
CRYO (n=67) |
|
COMBINED (n=69) |
|
P-value |
|
No recurrence (n=11) |
Recurrence
(n=56)
|
No recurrence
(n=25)
|
Recurrence
(n=42)
|
No recurrence
(n=38)
|
Recurrence
(n=31)
|
|
| Age (years) |
59±11 |
61±12 |
57±10 |
55±11 |
58±10 |
60±12 |
0.706 |
| Male |
8 (73%) |
34 (61%) |
16 (64%) |
32 (76%) |
24 (63%) |
16 (52%) |
0.968 |
| AF duration (months) |
60
(IQR 27-84)
|
60
(IQR 24-96)
|
36
(IQR 24-120)
|
61
(IQR 24-120)
|
60
(IQR 25-96)
|
84
(IQR 24-132)
|
0.063 |
| LA diameter (mm) |
43±5 |
43±5 |
43±4 |
42±5 |
43±4 |
42±4 |
0.736 |
| Hypertension |
2 (18%) |
19 (34%) |
12 (48%) |
13 (31%) |
10 (26%) |
16 (52%) |
0.506 |
| DM |
1 (9%) |
4 (7%) |
1 (4%) |
3 (7%) |
4 (11%) |
1 (3%) |
0.323 |
| IHD |
1 (9%) |
5 (9%) |
3 (12%) |
3 (7%) |
4 (11%) |
1 (3%) |
0.353 |
| Cardiac failure |
2 (18%) |
2 (4%) |
1 (8%) |
6 (14%) |
5 (14%) |
3 (10%) |
0.509 |
| CVA/TIA |
0 (0%) |
6 (16%) |
3 (12%) |
2 (5%) |
21 (11%) |
5 (16%) |
0.970 |
| AADs failed |
2±1 |
2±1 |
2±1 |
2±1 |
2±1 |
2±1 |
0.420 |
Patient characteristics in each group stratified by AF recurrence after a single procedure. Data shown as mean ± SD, median (IQR), or proportion (%) as appropriate. P-values shown are of univariate analysis assessing association of factors to recurrence of AF/AT.
Primary Endpoint: Freedom from AF/AT after a single procedure
Kaplan-Meier curves demonstrating freedom from AF/AT after a single procedure are shown in [Figure 1A]. At 5 years, 57% of COMBINED patients remained free of AF/AT after a single procedure compared to 47% CRYO and 19% RF patients (p<0.001 COMBINED vs RF and CRYO vs RF; p=0.043 COMBINED vs CRYO). At final follow-up, 38/69 (55%) COMBINED patients remained free of AF/AT compared to 25/67 (37%) CRYO and 11/67 (16%) RF patients. The COMBINED approach was superior to both RF (hazard ratio for AF recurrence, HR 0.33 95% CI 0.21-0.51) and CRYO (HR 0.63, 95%CI 0.39-0.99). CRYO in turn was superior to RF (HR 0.48, 95%CI 0.32-0.72).
Figure 1. . Comparison of AF free survival.
Kaplan–Meier analysis of survival free from AF following (A) index procedure
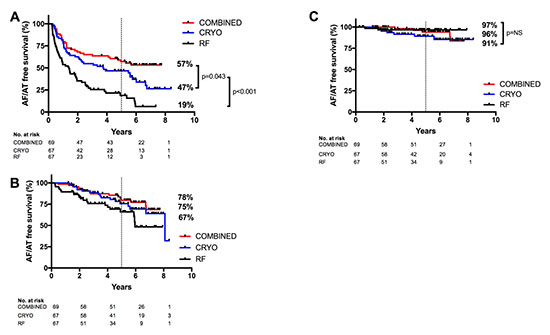
Secondary Endpoint: Freedom from AF/AT after one or more procedures
36/67 (54%) RF and 33/67 (49%) CRYO patients underwent one or more repeat procedure(s) compared to only 16/69 (23%) in the COMBINED group (p<0.01 for COMBINED vs RF and COMBINED vs CRYO) [Figure 2]. First repeat procedure was performed at median of 382 days (IQR 199-718 days) from index procedure with no significant differences between groups.
Figure 2. Number of AF ablation procedure(s). Number of AF ablation procedure(s) performed in each group.
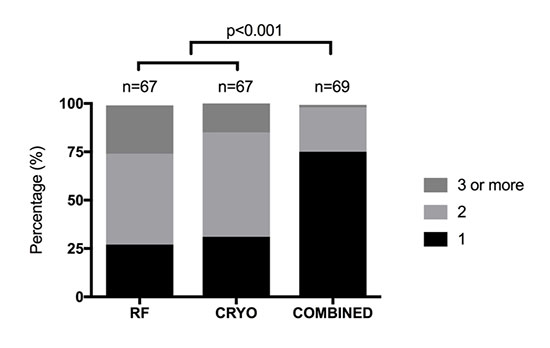
After a mean of 1.7 procedures in the RF and CRYO groups, and 1.3 procedures in the COMBINED group, 45/67 (67%) RF, 50/67 (75%) CRYO and 54/69 (78%) COMBINED patients remained free of AF/AT off antiarrhythmic drugs (RF v COMBINED, p=0.02; RF v CRYO, p=0.10; CRYO v COMBINED, p=0.80). After repeat procedure(s) at a median of 5 years, the COMBINED group remained superior to RF (HR 0.48, 95%CI 0.25-0.92). There were no significant differences between COMBINED vs CRYO (HR 0.80, 95%CI 0.40-1.60) and CRYO vs RF (HR 0.60, 95% CI 0.32-1.13) [Figure 1B].
When patients who remain symptom free on antiarrhythmic medications are included, the efficacy after repeat procedure(s) rise to 65/67 (97%) for RF, 61/67 (91%) for CRYO and 66/69 (96%) for COMBINED (p=0.20 COMBINED vs RF; p=0.15 CRYO vs RF; p=0.75 COMBINED vs CRYO) [Figure 1C].
There were significantly more patients in the RF group on antiarrhythmic medications compared to patients in the CRYO and COMBINED group: RF 20/67 (30%) vs CRYO 9/67 (13%) and COMBINED 10/69(14%), p-0.04. There was 1 death in the RF group and 2 deaths each in the CRYO and COMBINED group. All deaths occurred more than 2 years after the index procedures.
Number and distribution of reconnected PVs during first repeat procedure
Among patients undergoing a first repeat procedure, 6/16 (38%) in the COMBINED group had no reconnected PVs compared to 2/33 (6%) in the CRYO group and 2/36 (6%) in the RF group (CRYO/RF versus COMBINED, p < 0.001). Patients in the COMBINED group also had fewer reconnected PVs (mean number of reconnected PVs in the COMBINED group 1.2 vs 2.3 CRYO and 2.4 RF, p=0.034). [Figure 3].
Figure 3. Number of reconnected PV(s) during repeat procedure(s).Number of reconnected PV(s) documented during first and subsequent repeat procedure(s).
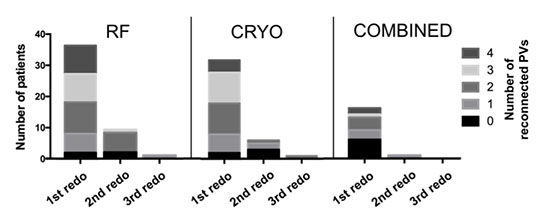
At the last procedure, 5/33 (15%) in the CRYO, 4/36 (11%) in the RF and 6/16 (38%) in the COMBINED group had no reconnected PVs.
Distribution of reconnected PVs and sites of PV reconnection during first repeat procedure
The distribution of reconnected PVs and sites of PV reconnections in each group is shown in [Figure 4].
Figure 4. Pattern of PV reconnection during first repeat procedure.Distribution of PV reconnections during the first repeat procedure. Number in the centre circle of each vein represents the frequency of the vein being reconnected expressed as a percentage of the total number of patients in each group. Numbers in the periphery show the distribution of reconnection sites within each vein among the subset of patient for which this was prospectively evaluated. S- superior, A- anterior, I- inferior, P- posterior.
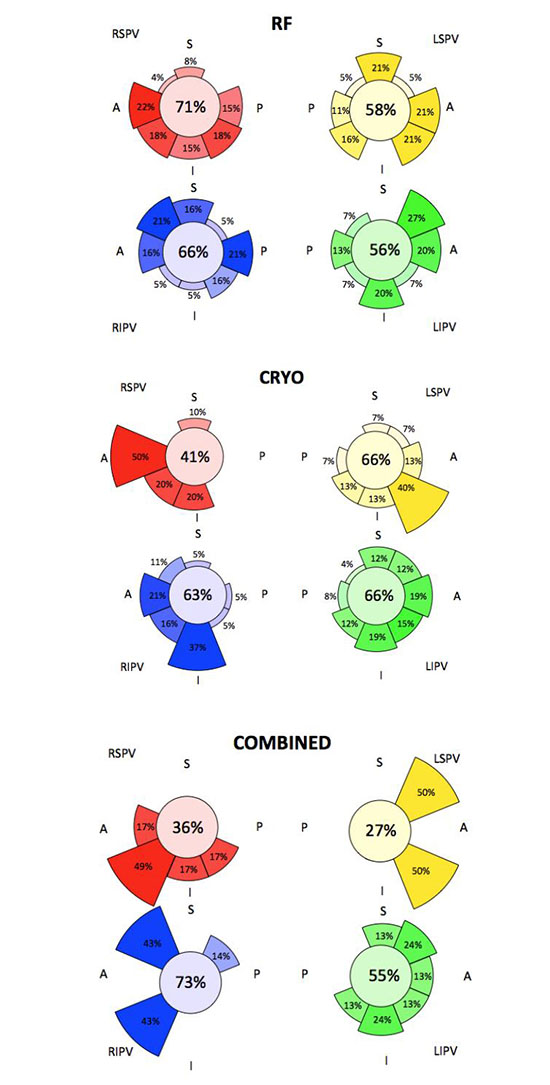
There was a significant difference between the groups in the rate of reconnection among the superior veins between the groups. For RSPV, both CRYO and the COMBINED groups had significantly less reconnection compared to RF (CRYO vs RF, OR 0.28 CI 0.10 – 0.75, p=0.015; COMBINED vs RF, OR 0.13 CI 0.03-0.47, p=0.001). For LSPV, there was significantly less reconnection in the COMBINED group compared to both CRYO and RF (COMBINED vs CRYO, OR 0.11 CI 0.03-0.48, p=0.002; COMBINED vs RF 0.16 CI 0.04-0.63, p=0.008). The frequency of PV reconnection in the inferior veins was similar between the groups.
PV reconnection sites were prospectively studied in a subset of 20 consecutive cases each in the CRYO and RF groups, and 10 in the COMBINED groups. There were 72 reconnection sites in 51 PVs in the CRYO group, 80 reconnection sites in 58 PVs in the RF group, and 23 reconnection sites in 19 PVs in the COMBINED group.
For the CRYO group, the anterior-inferior region (anterior, anterior inferior and inferior segments) accounted for 43 out of 63 sites (68%) where reconnection was found, compared to only 33 out of 81 sites (41%) in the same region in the RF group (P= 0.001). This pattern is most pronounced in the RSPV where 90% of reconnection occurred and least so in the LIPV where only 53% was accounted for.
For the RF group, the superior and inferior regions on the right sided veins (anterior superior, superior and posterior superior segments of the RSPV and anterior inferior, inferior and posterior inferior segments of the RIPV) were least likely to be reconnected, accounting for only 9 out of 45 (20%) of reconnected right sided PVs. For the left sided veins, there were no reconnection sites on the inferior segment of LSPV and superior segment of LIPV. The sites of reconnections were otherwise evenly distributed when assessing segments within one clock face of each other.
For the COMBINED group, the pattern of reconnection in the RSPV appears similar to the CRYO group with 5 out of 6 (83%) of PV reconnections occurring in the anterior-inferior region. Otherwise, the inferior veins were more likely to be reconnected, accounting for 17 of the 26 segments (65%) with no clear pattern of distribution.
This study reports the 5-year outcome of three different PVI strategies for PAF: the cryoballoon, radiofrequency catheter ablation (RFCA) or a novel combined approach. We found that after a single procedure, the combined approach resulted in a significantly lower rate of AF recurrence in the long term compared to both cryoballoon and RFCA, and cryoballoon was in turn superior to RFCA. The combined approach was associated with significantly fewer reconnected PVs compared to the other two groups. The pattern of PV reconnection differed between those who underwent cryoballoon compared to those undergoing RFCA and may explain the synergistic effect of the combined approach. After repeat procedure(s), efficacy was similar between the groups with AF free survival of ~70-80% at 5 years off antiarrhythmic medications although the combined approach remained superior to RFCA. This combined with the proportion of patients with recurrence despite no PV reconnection suggest that even the perfect PVI strategy will have a long-term ceiling of ~80% success due to non-PV triggers.
Long term efficacy of the cryoballoon ablation
We have previously shown in a randomised controlled trial that the single procedure success rate off antiarrhythmic drugs at 1 year was 67% following ablation with the first generation cryoballoon[6], which was in keeping with other randomized studies and registry data[4,8,10]. The current study shows that at median follow-up of 5 years, AF free survival following cryoaballoon ablation drops to 47%.
There is limited long term (over 1 year of follow up) data for cryoballoon ablation in the literature. Vogt et al reported the outcomes of 605 patients who underwent cryoballoon ablation in a prospective registry [10]. Similar to our study, both 23 and 28mm Artic Front cryoballoons were used and Freezormax catheter was used when isolation was not achieved using the cryoballoon(s) alone. At 1 year follow-up, AF free survival after a 3-month blanking period was around 70%. At median follow-up of 30 months, follow-up data were available for 451 patients with 62% remaining free of AF. One other observational study involving 139 patients reported 49% freedom from AF at mean follow-up of 457 days [11]. Our findings are consistent with these data.
Comparison of long term single procedure efficacy to RF and Combined approach
The 1-year success rate obtained with conventional RF ablation was 47% and this dropped to 19% at median follow-up of 5 years. Recent multicenter trials and a large prospective registry have reported single-procedure success rates off antiarrhythmic drugs in the region of 43-50% at up to 2 years follow-up[2,12]. The results obtained with RF ablation in the current study therefore seem to be consistent with ‘real world’ practice. Cryoballoon ablation has a higher single-procedure AF free survival rate at 5 years, suggesting greater durability of PV isolation with this technology.
In contrast, AF-free survival for patients who had the combined approach was 57% during long-term follow-up. This suggests a lower rate of attrition compared to the other 2 groups and is comparable to other studies looking at rates of late recurrence [13].
We have previously suggested that the combined approach may be cost-effective over the long term by reducing the number of repeat procedures needed [14] but further study with appropriate economic modeling will be required to answer this question.
Patterns of PV reconnection comparing cryoballoon and RF ablation
We found a significantly different pattern of PV reconnection between the cryoballoon and RF group. Firstly, the RSPV appears to be less likely to be reconnected following cryoballoon ablation. Secondly, the anterior-inferior region appears more likely to be reconnected in patients undergoing cryoballoon ablation.
With the exception of Van Belle [11], other centers have also reported a lower incidence of PV reconnection of the RSPV following cryoballoon ablation with the left sided veins more likely to be reconnected than the right [4,15,16].
We are aware of only two studies which have characterized the pattern of PV reconnection sites within each vein following cryoballoon ablation. The first by Ghosh et al [17] studied 51 repeat procedures at a mean of 9 months following cryoballoon ablation. The study found that the anterior segments of the left-sided veins and the inferior segment of the RIPV was most likely to be reconnected.
Kuhne et al compared the pattern of PV reconnections between cryoballoon and RF ablation [18]. They reported the PV reconnection sites in a cohort of 25 patients with PAF undergoing cryoballoon ablation compared to 25 age and sex matched controls who underwent conventional RF ablation. After a 3-month blanking period, 5(20%) patients in the cryoballoon group and 7 (28%) patients in the RF group underwent a repeat procedure with a mean of 3 reconnected PVs per patient in each group. Similar to our findings, there were significantly fewer reconnected RSPVs and PV reconnections occurred most frequently in the inferior regions of the veins. It is important to note that in this study repeat procedures were performed within 1 year of the index procedure compared with the longer follow-up duration in our study. It remains uncertain whether PV reconnection and gaps become more or less apparent over time or simply remain unaltered.
PV reconnections in the Combined approach
The striking finding in our study is the low long-term recurrence rate and the low number of reconnected PVs in the patients in whom AF recurs in the combined group. This is the first long term report we are aware of for such an approach.
There are theoretical advantages to PV isolation by either segmental ostial isolation or WACA. The use of these two modalities in combination to create two rings of scar to insulate the PVs may therefore draw on the advantages of each strategy. In addition, the concomitant use of radiofrequency and cryothermal energy may itself be synergistic [19].
By studying the patterns of PV reconnection sites, we postulate another mechanism for the synergistic effect of the combined approach. Segmental ostial isolations using cryoballoon and WACA lines using RF appear to result in different patterns of PV reconnection. By combining the two approaches, the ‘vulnerable’ sites associated with each modality are covered by the other complementary technique.
Finally, 18% of patients overall who underwent a repeat procedure were found to have all PVs isolated. Furthermore, 9% of the whole combined cohort (6/69) had recurrent AF but were found to have all four PVs isolated at the repeat procedure. This is therefore a minimum proportion of patients that have non-PV triggers [20]. It is probable that some patients (in all groups) had bystander PV reconnection, although this is not clear until patients have a repeat procedure with all PVs isolated. This leads us to conclude that 10-20% have non-PV triggers that may play a significant role in PAF and suggests a likely ceiling on the long-term success rate of a PVI alone strategy for PAF of 80-90%.
Although this study was conducted at an experienced high-volume unit, the success rates in the conventional RF ablation group were seemingly average for the literature but comparable to real world outcomes [21,22,23]. In addition, follow-up was guided primarily by symptoms and hence asymptomatic recurrences of AF may have been missed. However, this again reflects real world practice [2], and equally affects all three groups of patients.
Contact force sensing technology is now available, as is the second generation cryoballoon with short to medium term outcomes comparing the two being reported [10]. It remains to be seen whether these advances or others will substantially impact long term success rates.
Although this study reports the outcomes of a previous generation technology, the results demonstrate that there appears to be a ceiling on long-term success with PVI alone strategy regardless of initial technique used and after repeated procedures.
We have shown that the 5-year outcome following a single catheter ablation procedure for PAF using a combined approach of RFCA followed by cryoballoon ablation is superior to that of either technique alone. Ablation with the cryoballoon was also superior to RFCA. The pattern of PV reconnection differs between cryoballoon and RFCA, which may explain the synergistic effect of the combined approach and low rates of PV reconnection at repeat procedures. These data suggest an excellent outcome at 5 years with an effective PVI strategy for PAF. However, the long-term success rate with such an approach is likely have a ceiling of 80-90% due to non-PV triggers.