Anticoagulation After Catheter Ablation of Atrial Fibrillation: Is it time to Discontinue in Select Patient Population?
Varunsiri Atti1, Mohit K Turagam2, Juan F. Viles-Gonzalez3, Dhanunjaya Lakkireddy4
1
Michigan State University-Sparrow Hospital, East Lansing, MI..2
Helmsley Electrophysiology Center, Icahn School of medicine at Mount Sinai, New York City, NY..3
Heart and Vascular Institute, Tulane University School of Medicine, New Orleans, LA..4
Kansas City Heart Rhythm Institute, Kansas City, KS..
Catheter ablation is an effective strategy for treatment of drug-refractory atrial fibrillation (AF). Continuation of oral anticoagulation (OAC) beyond 3 months after an apparently successful ablation of AF remains controversial.
A systematic electronic search of the scientific literature was performed in PubMed, EMBASE, SCOPUS and Google Scholar. Studies comparing continuation vs discontinuation of OACs after an apparent successful ablation of AF among patients with CHA2DS2VASC or CHADS2 score ≥2were included. Clinical outcomes included cerebrovascular events, systemic thromboembolism and major bleeding. Risk ratios (RR) and 95% confidence intervals for above outcomes were calculated.
Nine observational studies were eligible and included 3,436patients of whom 1,815 continued OACs and1,621 discontinued OAC post –AF ablation. There was no significant difference in risk of cerebrovascular events (RR: 0.85, 95%CI: 0.42 to 1.70, p= 0.64)and systemic thromboembolism (RR: 1.21, 95%CI: 0.66 to 2.23, p= 0.54)between the two groups. Continuation of OACs was associated with an increased risk of major bleeding (RR: 6.50, 95% CI: 2.53 to 16.74, p= 0.0001).
In conclusion, discontinuation of oral anticoagulation 3 months after a successful AF ablation appears to be safe in highly selected closely monitored patients. Further randomized trials are warranted to assess the safety of discontinuing OACs after AF ablation.
Key Words : Atrial Fibrillation Ablation, Oral Anticoagulants, Cerebrovascular Accident, Systemic Thromboembolism, Bleeding.
Correspondence to: Varunsiri Atti,
Clinical center, 788 Service road
East Lansing, MI,
Catheter ablation of atrial fibrillation (AF) emerged as an effective treatment strategy for symptomatic, drug-refractory AF with an estimated success of 65-90% for paroxysmal AF[1]. Although prior studies have demonstrated a reduction in the risk of stroke/systemic thromboembolism after an apparently successful AF ablation, there is limited evidence to suggest that the risk is completely eliminated[2,3].Hence,current guidelines recommend caution against discontinuation of oral anticoagulation (OAC) post-AF ablation in patients with a CHA2DS2VASC score ≥2[4].Regardless of the benefits, continuation of OAC is not completely benign and is associated with an increased risk of adverse events such as major bleeding and mortality. In addition, non-compliance and high economic burden prevents the wide-spread use of OAC in eligible patients. Due to lack of randomized controlled trials, we sought to perform a meta-analysis of all the studies published to date to evaluate the safety and efficacy of continuation vs. discontinuation of OACs after an apparently successful AF ablation in patients with or CHADS2 or CHA2DS2VASC score≥ 2.
A systematic search of PubMed, EMBASE, SCOPUS and Google Scholar from inception to November1st 2018 was performed. We used the following keywords: “atrial fibrillation ablation,” “AF ablation” “anticoagulation,” “warfarin,” “novel oral anticoagulants” and“NOAC”. The reference lists of original studies, conference abstracts and relevant review articles were further reviewed. We included studies that reported clinical outcomes comparing continuation vs. discontinuation of OAC in patients with CHA2DS2VASC or CHADS2 score ≥ 2 who underwent AF ablation. Two investigators (V.A and M.K.T) independently performed the literature search, reviewed the originally identified titles and abstracts and selected studies for pooled analysis based on the inclusion criteria. The quality of each study was assessed using the Newcastle Ottawa scale. We evaluated the following clinical outcomes: 1) cerebrovascular events (CVE), 2) systemic thromboembolism, and 3) major bleeding. Statistical analysis was performed using random-effects model estimating the risk ratio (RR) and 95% confidence interval (CI) obtained by Mantel-Haenszel method.Heterogeneity was assessed using Higgins and Thompson's I2 statistic, with I2 values <25%, 25% to 50%, and >50% corresponding tomild, moderate and severe heterogeneity respectively[5]. Analysis was performed using Cochrane Collaborative software, RevMan 5.3.
Nine observational studies met our inclusion criteria [2,3,6-12]. Among 3,436 patients, 1,815 continued OACs and 1,621 discontinued OAC post – AF ablation. The OACs were discontinued at 3-8 months post procedure. The follow-up period ranged from 12 – 60 months. Monitoring of AF varied widely and included 24 hour, 7 days and 30 days cardiac monitoring. [Table 1] summarizes the baseline characteristics of the included studies. There was no significant difference in the risk of CVE(RR: 0.85, 95%CI: 0.42 to 1.70, p= 0.64)and systemic thromboembolism (RR: 1.21, 95%CI: 0.66 to 2.23, p= 0.54) between the two groups. Continuation of OAC was associated with a significantly higher risk of major bleeding (RR: 6.50, 95% CI: 2.53 to 16.74, p= 0.0001), [Figure 1]. Test of heterogeneity was low risk for all the clinical outcomes (I2= 0%).
Figure 1. Forest plot for study outcomes (Figure 1.1.Cerebrovascular event (CVE)).
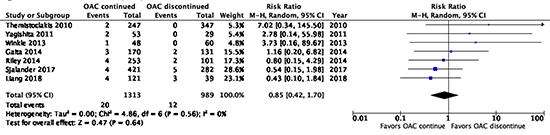
Figure 1.2. Systemic thromboembolism
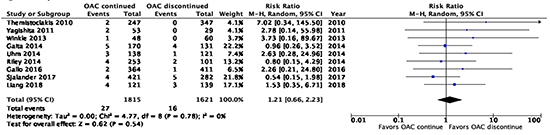
Figure 1.3. Major bleeding
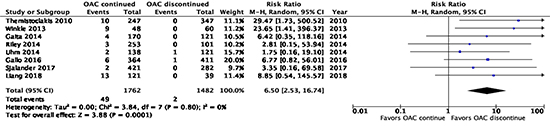
Table 1. Baseline characteristics of included studies
| Study |
Design |
Type of AF |
Study period |
Type of OAC |
Mean ± SDCHADVASC Score or CHADS2 Score |
Mean duration of OAC |
Sample size
OAC OACContdiscont |
Mean age ± SD(years)
OAC cont vs OAC discontinued |
Type of ablation performed (Pulmonary vein isolation (PVI) +/- additional ablation) |
Follow-up period |
AF monitoring |
| Liang, 2018 |
Retrospective |
Persistent 50%; Long standing- 16.7% |
2004-2012 |
Warfarin, Dabigatran, Rivaroxaban |
2.2 ± 1.5 |
NR |
121 |
39 |
61.5 ± 10.2 vs 58.7 ± 8.8 |
PVI + non-PV trigger ablation |
3.6 ± 2.4 years |
Continuous monitoring 30-day post ablation, 30-day telemetry at 6-months and 1-year. |
| Sjalander, |
Retrospective |
NR |
2006-2012 |
Warfarin |
2.8 ± 1 |
3 months |
421 |
106 |
59 ± 9.4 |
PVI |
2.6 years |
NR |
| Gallo, 2016 |
Retrospective |
Paroxysmal 50.8% Persistent 49.2% |
2003-2011 |
Warfarin |
2.1 ± 1.1 |
3 months |
364 |
411 |
64 ± 8 vs 60 ± 10 |
PVI |
60 ± 28 months |
24hour holter ECG monitor every 6 months |
| Riley, 2014 |
Retrospective |
Paroxysmal 65.6%; Persistent 28%; Long standing 6.4% |
2000-2009 |
Warfarin |
NR |
NR |
253 |
101 |
60±9.6 vs 55 ± 11 |
PVI |
60 ± 28 months |
PVI + non-PV trigger ablation |
1 year |
30-day trans-telephonic monitor. Repeat trans-telephonic monitor at 6 and 12 months. Echo at 6-weeks. |
| Gaita, 2014 |
Retrospective |
Paroxysmal 42.6%; Persistent 57.4% |
2001-2009 |
Warfarin |
NR |
3 months |
170 |
131 |
61±10 vs 57±11 |
PVI for paroxysmal AF; linear lesions forredo-procedures; PVI + ‘7’ scheme for persistent AF |
60.5 months |
24hour/7day holter monitor at 1,3,6 months and ICD interrogation (2%) |
| Uhm, 2014 |
Retrospective |
Paroxysmal 75.4% Persistent 24.6% |
2009-2011 |
Warfarin |
2.82 ± 0.98
vs2.78 ± 1 |
7.3 months |
NR |
138 |
121 |
62.9 ± 9 vs 65.5 ± 8.3 |
PVI+/-linear ablation or complex fractionated atrial electrogram |
18 ± 12.2 months |
Outpatient follow up at 1 month and then every 3 months for 1 and then every 6 months. Holter monitor at 3,6,12,18 and 24 months. |
| Winkle, 2013 |
Retrospective |
Paroxysmal 37%; Persistent 46.3%Long standing 16.7% |
2003-2011 |
Warfarin |
4.1 ± 1.4 |
7.3 months |
48 |
60 |
NR |
PVI + ablation in the coronary sinus and/or right atrium and superior vena cava isolation |
2.2 ± 1.3 years |
Daily ECG strips for 1-3 months. ECG monitor for 7-21 days at 3 months. Echo and 24hour ECG at 1 year. |
| Yagishita, 2011 |
Retrospective |
Paroxysmal 69.1%Persistent 30.1% |
2003-2006 |
Warfarin |
NR |
3 months |
53 |
29 |
NR |
PVI + Cavotricuspid isthmus ablation |
44 ± 13 months |
Outpatient follow-up at 1,3 and 6 months. 24hour holter monitor at 3,6 and 12 months. |
| Themistoclakis, 2010 |
Retrospective |
Paroxysmal 59%;
Persistent 19%;
Long standing 22%
|
2003-2005 |
Warfarin |
NR |
5 ± 3 months |
247 |
347 |
57±11 vs 57±11 |
PVI; PVI + linear lesions, ablation of complex fractionated elctrograms, isolation of superior vena cava |
28 ± 13 vs 24 ± 15 months |
ECG within 1 month. Holter monitor at 1,3,6 months. Trans-telephonic monitoring |
*Median (IQR).
The important findings of our study include the following: Among patients with a CHA2DS2VASC or CHADS2 score ≥2 who underwent an apparently successful AF ablation, 1) there was no significant difference in the risk of CVEor systemic thromboembolism with continuation vs discontinuation of OACs after 3 months. 2) Discontinuation of OACs was associated with a substantially lower risk of major bleeding. A search between 2016 and 2018 in PubMed identified 2 other systematic reviews and meta-analyses that also found no significant increased risk of CVE/systemic thromboembolism but increased risk of major bleeding with long-term continuation of OAC after a successful AF ablation procedure[13,14]. In contrast to these prior meta-analysis, we only included studies with patients who had CHA2DS2VASC or CHADS2 score ≥2 representing a high-risk cohort of patients.
Several published studies support the notion that maintenance of sinus rhythm can effectively reduce the morbidity associated with systemic thromboembolism, obviating the need for long-term OAC[15].Catheter ablation is associated with endothelial denudation, atrial stunning and activation of coagulation cascade paradoxically increasing the risk of systemic thromboembolism in the short-term requiring treatment with OAC for at least 2-3 months. However, the risk of bleeding associated with further continuation of OACs outweigh the benefits of stroke prevention in low risk patients (CHA2DS2VASC<2) post-AF ablation and there is little dispute about stopping OAC in this group of patients[16].However, patients with a high risk of stroke (CHA2DS2VASC score ≥2) also have high risk of major bleeding and continuation of OAC can be associated with a higher risk of adverse events as demonstrated by our study results. This practice is reflected in a recent survey by the writing group of 2017 professional medical society guidelines that about 1/3rd of patients with CHA2DS2VASc score≥ 2 discontinued OAC beyond two months post – AF ablation.4Such high risk of major bleeding is not a benign finding as patients with high CHA2DS2VASC also have high HAS – BLED scores and are prone to increased risk of all – cause mortality and cardiovascular mortality as demonstrated in prior studies[17].
Currently, two RCTs of discontinuation of OAC post-AF ablation are underway. OAT trial (Safety of OAC Therapy Withdrawal After Successful Cardiac Ablation in Patients with AF and Associated High Risk Factors for Embolic Events trial, Clinical trials.gov NCT01959425) is randomly assigning patients who underwent catheter ablation and remain AF recurrence-free will be randomized to OAC withdrawal group or the OAC group. The primary endpoint is occurrence of any major systemic thromboembolic event and, is estimated to be completed in December, 2019. OCEAN trial (Optimal AC for Higher Risk Patients Post-Catheter Ablation for AF trial, Clinical trials.gov NCT02168829) is investigating whether long-term OAC (rivaroxaban 15 mg daily) is superior to antiplatelet therapy (Aspirin 75-160 mg), alone in preventing CVE in moderately high-risk patients following successful AF ablation. The primary endpoint is the composite of stroke; systemic embolism and embolic stroke as detected by brain MRI and, is estimated to be completed in December 2021.
First, majority of the studies performed was in the warfarin era, the use of NOACs could substantially reduce the risk of major bleeding but the risk is not completely eliminated. Second, there were differences in the risk profile of study participants among the included studies. Third, there is a risk of bias as the studies included were observational and non-randomized. Fourth, the time frame of discontinuation of OAC ranged from 3-8 months and was at the discretion of the physician. Fifth, publication bias could not be assessed as the number of included studies is <10. Sixth, episodes of silent AF can be underestimated due to lack of continuous cardiac monitoring on follow up. Despite these limitations,our analysis provides valuable insight regarding the use of OACs after an apparent successful ablation of AF.
In conclusion, discontinuation of oral anticoagulation 3 months after a successful AF ablation appears to be safe in highly selected closely monitored patients. Further randomized trials are warranted to assess the safety of discontinuing OACs after AF ablation.