Atrial Fibrillation Associated with Heart Failure, Stroke and Mortality
Stefano Bordignon MD1, Maria Chiara Corti MD, MHS2, Claudio Bilato MD, PhD1
1Division of Cardiology, Department of Cardiac, Thoracic and Vascular Sciences, University of Padova.2Division of Primary Care, Local Health Unit 16, Veneto Region, Padova, Italy.
Atrial Fibrillation (AF) is the most common arrhythmia in the western world. Because AF prevalence rises with age and western populations are increasingly aging, AF has been called a “growing epidemic”, especially among older persons, with social and economic consequences. AF may concur to disability and may cluster with other co-existing clinical conditions. AF is an independent risk factor for stroke by increasing the thromboembolic risk profile and is associated with heart failure severity. Among persons with AF, prevalence of stroke, coronary heart disease, peripheral artery disease, cognitive impairment and physical disability is significantly higher. AF is associated with higher risk of mortality through the association with stroke and heart failure: ischemic strokes are more severe if AF is present and AF may represent a marker of more severe heart failure. Independently of other known predictors of mortality, death rates are almost doubled by AF. AF, therefore, is a considerable source of morbidity and mortality, is associated with disability, and is a major determinant of quality of life.
Correspondence to:
Claudio Bilato MD, PhD, Division of Cardiology, Department of Cardiac, Thoracic and Vascular Sciences, University of Padova, Via Giustiniani 2, Italya, PA 19104.
Atrial fibrillation (AF) is the most common cardiac arrhythmia in the western world, with a reported prevalence of 1-2% in the general population, i.e. from 4 to 6 millions affected subjects in the US and European populations, respectively. In addition, many cases of AF remain undiagnosed because of lack of symptoms (silent AF) and, therefore, the true prevalence of AF is probably even higher.1
Several large population studies have analyzed both prevalence and incidence of AF in the general population. In the Framingham heart study, for example, a biennial examination of more than 5,000 patients, aged 28–62 years and free of cardiovascular disease, showed that both prevalence and incidence rose with age, with a 2% increase of probability that AF would develop every two decades.2 In the Renfrew/Paisley study, more than 15,000 middle aged (45-64 years) adults in Scotland were enrolled in the mid seventies and followed up for 20 years. The baseline prevalence of AF was 0.65%, while the AF-related hospitalization rate was of 2.1 and 1.7/1000 person-years in men and women, respectively.3 In another European study, the Rotterdam Study, a more heterogeneous cohort of 6,808 subjects 55 years and older was studied. The prevalence in the middle-aged subgroup (55-59 years old) was only 0.7%, but it rose up to 17.8% in patients aged 85 years and older, with an overall prevalence rate of 5.5%. During follow up (6.9 years), the incidence of newly discovered AF in the cohort was 9,9/1000 subjects per year and increased from 1,1/1000 patients-year in the younger group to 20,7/1000 patients-year among older subjects (80-85 years old).4
More recently, our group analyzed a cohort of patients aged 65 years and older, selected in northern Italy with an age-sex stratified sampling strategy. Overall, our results showed a weighted AF prevalence of 7,4% which increased with advancing age (from 3.6% to 9.2% and to 17% in the 65-74 years old, 75-84 years old, 85 years and older subjects, respectively). During a 4-year follow up period, an incidence rate of 6/1000 person-years in the 65 to 74 years decade and 14/1000 person-years both in subjects 75 to 84 and 85 years and older was recorded.5
Prevalence and incidence of AF in the general population was also measured using the data of the Olmsted County (Minnesota) population.
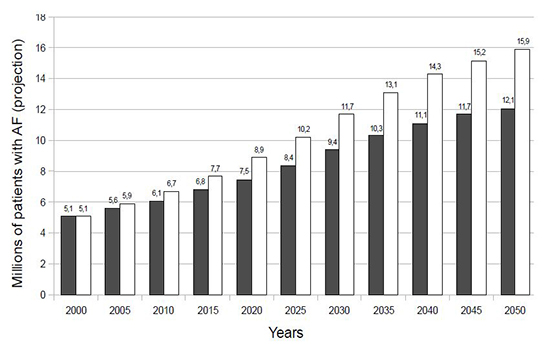
Between 1980 and 2000, AF was diagnosed in 4,618 subjects by electrocardiogram. The weighted AF incidence was 3,04/1000 person-years in 1980, and rose up to the 3,68/1000 person-years in the year 2000, with a relative increase of 12,6%. Based on this observation, a prevalence model estimated in the total U.S. population an AF prevalence of 2,1% in the 1980s and of 2,5% in the year 2000. The same model, applied to the demographic projections for the U.S., predicted an estimate of 12,1 millions AF patients in 2050, but this number rose up to 15,9 millions when applying the increased incidence rate observed between 1980 and 20006 (Figure 1).
Figure 1. Prevalence Estimates of AF in the US Population with (white columns) and Without (grey columns) Taking in Account the Increase in Incidence Observed Between 1980 and 2000. Data from Reference.6
Atrial Fibrillation and Heart Failure
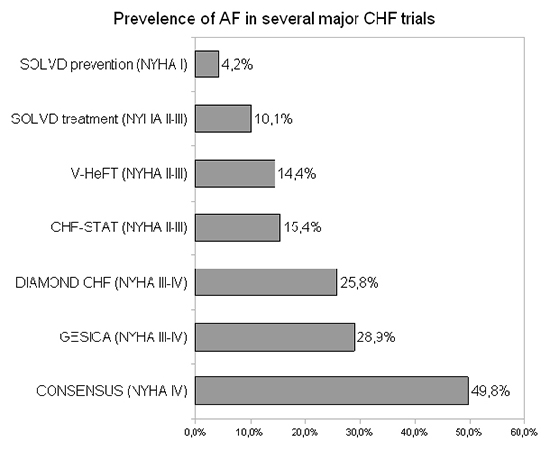
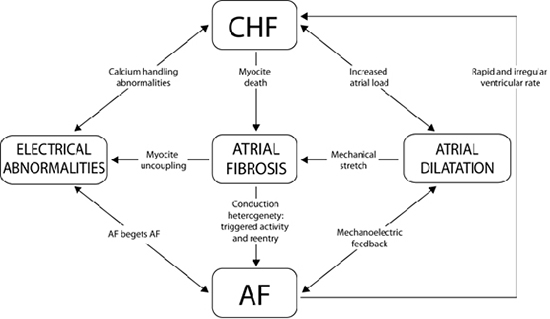
In clinical trials and observational studies, the prevalence of AF among congestive heart failure (HF) patients varies from 10 to 50%, depending on the HF severity: it is about 10-15% in patients with II-III NYHA classes and rises up to 50% in severe congestive HF (NYHA IV)7,8(Figure 2). Both diastolic and systolic HF result in a high risk of AF, as a consequence of several conditions such as increased atrial loading, atrial dilation, conduction disturbances, and atrial fibrosis.9 In addition, AF can lead to HF because of higher heart rate and subsequent tachycardiomyopathy.10 As observed in animal models, the mechanisms involved in this complex process seem to be related to myocardial energy depletion, myocardial ischemia, abnormalities of calcium regulation, and/or extracellular matrix remodeling.11
HF can trigger AF through the myocardial stretch associated with the increased atrial loading. When the pressure of the left atrium increases, activation of stress-stimulated channels, secretion of Angiotensin II, and generation of other endocellular signals, induced by adrenergic and muscarinic receptors, all occur. The result is an increased level of the endoplasmic calcium, which alters the atrial electrophysiology because enhances the automaticity and the triggered activity of the myofibrils, especially in regions like the pulmonary veins ostia, leading to AF. HF also concurs to sustain the arrhythmia by activating the apoptotic cascade, with consequent fibroblast proliferation, myocardial fibrosis, and “structural remodeling” of the atria.12 The interactions between AF, HF, and atrial fibrosis are summarized in Figure 3 and have been described elsewhere.9
The clinical and prognostic relationships between AF and HF have been investigated in several trials and clinical studies, often with conflicting results. Mamas et al. described the impact of AF on mortality in patients with congestive HF, metaanalyzing data from randomized trials and observational studies. Among the 30,248 patients with congestive HF included in the analysis, 4,141 were in AF and 26,107 in sinus rhythm. In multivariate analysis, AF was associated with a 40% increase in the relative risk of mortality (OR=1,4; 95%CI=1,32-1,48). When only the 9 observational studies (n=23,721) were considered, AF confirmed its significant association with mortality with a pooled OR of 1,14 (95% C.I. 1.03-1,26). 13
When subgroups of HF patients with impaired or preserved LV systolic function were considered, no significant differences were observed on the effect of AF on mortality. By contrast, Linssen et al. focusing on 927 patients with stable HF, observed that, after 18 months of follow up, AF was an independent predictor of combined mortality and hospitalization (OR 1,49; 95% CI 1,04-2,14) only in HF patients with preserved ejection fraction (EF) as compared to patients with low EF.14 These contrasting observations could be explained by a possible collinearity between HF and AF, as suggested by data from the Pro.V.A. study.5 In this study, the association between HF and AF was very strong and the presence of HF was associated with a fivefold increase in the risk of AF (OR 5.09, 95% CI 3.20 to 8.11), supporting the hypothesis that HF and AF in the same mortality model could generate collinearity.
Interestingly, some studies found a different influence of AF and HF on mortality with respect to their temporal relationship. The Euro Heart Failure survey studied 10,701 patients hospitalized because of incident HF: 3,673 had a pre-existing AF, while 1,001 showed a new onset AF. The study revealed that the occurrence of a new AF during hospitalization was associated with a 1.5-fold (95% CI, 1.1-2.0) increased risk of in-hospital mortality as compared to patients who did not present AF during hospitalization.15
Likewise, the Framingham Heart Study, analyzing the temporal relationships between AF and HF, showed that a late development of AF in HF patients increased the risk of mortality of 60% (HR 1.6; 95% CI, 1.2-2.1) among men and almost three times (HR 2.7;95% CI, 2.0-3.6) among women.16 A similar analysis was also conducted in the Olmsted County-Minnesota Cohort: among the 1,664 HF patients enrolled in the study, 553 presented prior history of AF and 384 subjects developed AF after HF. Over a median follow-up of 4 years, 450 deaths were observed among persons with prior AF, 314 among those with AF occurring after HF, and 572 among patients without AF. After adjustment, those with AF prior to HF had a 29% increased risk of death as compared to patients without AF, while those who developed AF after HF experienced a 2.2-fold increased risk of death.17
Management of AF (control of the heart rate or of the rhythm) in HF patients is still under debate. Several studies have shown no difference between rhythm and rate control strategies, although rhythm control has been associated with excellent survival if sinus rhythm could be maintained. Among these trials, the AFFIRM study confirmed that the presence of sinus rhythm was associated with a considerably lower risk of death with an HR of 0.53 (95% CI 0.39–0.72).18 However, among the 4,060 patients of the AFFIRM study, 23% had a history of congestive HF and, in this subgroup, none of the strategies demonstrated to be superior in lowering the mortality risk.
The AF-CHF trial investigated the differences between rate and rhythm control in 1,376 patients with history of AF and clinical HF or EF<35%. During the 37 months of follow up, there were no significant differences between the two strategies in the primary endpoint of cardiovascular death, although this lack of effect could be the result of a too small decrease in the prevalence of atrial fibrillation, as stated by the authors.19
The positive effect of antiarrhythmic drugs, the first line therapy to restore and maintain sinus rhythm, have been offset by an increase in death from non-cardiac causes.20 A fibrotic and remodeled atrium, a typical finding in congestive HF patients, has a lower response to antiarrhythmic drugs,12 with more detrimental side effects and less beneficial results. Therefore, new and safer therapeutic strategies are needed to improve the preservation of sinus rhythm in patients with congestive HF. In addition, whether catheter ablation will become an effective strategy is still under debate and not yet demonstrated, considering that the AF ablation seems to be less effective in highly fibrotic atria.21
According to the current guidelines for AF management, when a rate control strategy is chosen, beta-blockers are the first line therapy.1,22 As observed in the rate control arm of the AF-CHF trial19 and in other trials, beta-blockers are able to lower the prevalence and the incidence of AF.23 Beta-blockers are also the first line drug to reduce mortality and hospitalization of congestive HF patients, and are IA class treatment in the HF guidelines.24 However, it is worth noting that, in some trials contributing to this recommendation, such as the MERIT-HF and the CIBIS-II trials, beta-blockers showed no effect on mortality for patients with AF and congestive HF.25,26 Again, this lack of effect could be explained by AF being a marker of a more diseased heart or of a worse clinical condition.7 As already hypothesized in the Pro.V.A. study cohort, the strong association between HF and AF could explain the inability of HF to predict mortality. In other words, AF may identify the sickest HF patients with the worst prognosis, as compared to HF patients without AF, and play a dominant role in predicting mortality risk.5
Figure 2. Prevalence of AF in Congestive HF Trials, According to the NYHA Class of the Enrolled Population. Modified from Reference.8
Atrial Fibrillation and Stroke
AF is characterized by abnormal blood flow in the left atrium, often assessed at echocardiography as spontaneous echocontrast, and by other atrial wall abnormalities, such as atrial dilation, endocardial denudation and fibroelastic infiltration of the extracellular space. These abnormalities together with alterations of blood constituents, such as coagulation and platelet activation, inflammation and growth factor modifications, are responsible for the so called “Virchow triad revisited”, which represents the pathophysiological basis of the association of AF with stroke.27
AF is a major cause of stroke: in the German Stroke Data Bank, one fourth of the 5,017 acute ischemic strokes were found to be caused by cardioembolism.28 Because AF is often silent, it should be searched for in all ischemic strokes, not only by standard ECG at admission, but also by more sensitive methods. Jabaudon et al., for example, reported that out of one hundred forty-nine consecutive patients admitted to the neurology department because of acute stroke or TIA, standard ECG identified AF only in 2.7% of the cases at admission (4/149 patients) and in 4.1% of remaining patients within 5 days (6/145). However, ECG-Holter disclosed AF in an additional 5% of patients with normal standard ECG (7/139 patients), whereas an event loop recorder lasting 7 days detected AF in further 5.7% of the remaining patients with a normal standard ECG and normal ECG-Holter (5/88 patients).29
Figure 3. Pathophysiological Interactions Between AF and Congestive HF, Modified from Reference.9
Cardioembolic stroke patients seems to have a worse outcome as compared to non- cardioembolic stroke patients. The Copenhagen Stroke Study analyzed the clinical data from 1,197 patients and referred to a single center for ischemic stroke. AF was found in 18% of the patients. Among them, neurologic and functional outcomes were markedly poorer, as compared to patients with non- cardioembolic stroke, and this worse outcome was exclusively explained by the higher severity of the stroke.30 Similar data were observed by the Japan Multicenter Stroke Investigators, who recruited 15,831 subjects with ischemic stroke. In multivariate regression analysis, the proportion (21%) of patients with AF showed higher risk of severe stroke and premature death.31
The characteristics and/or the types (paroxysmal, persistent or permanent) of AF do not seem to affect the incidence rates of stroke. In the Stockholm Cohort of Atrial Fibrillation, for example, both paroxysmal and permanent AF doubled the risk of stroke as compared to the general population. With a standardized incidence ratio of ischemic stroke in patients with paroxysmal AF of 2.12 (95% CI 1.52–2.71), evidence was provided that all AF patients should receive a protective anticoagulant treatment.32
As reported above, AF-related stroke is often more severe and results in long-term disability or death. To this regard, it is worth remembering that only the antithrombotic therapy has been shown to reduce death due to AF-related strokes.1 In a cohort of 13,559 patients with non-valvular AF treated with oral anticoagulant (OAC), aspirin or no antithrombotic therapy, 618 strokes occurred between 1996 and 1999. Out of the 596 strokes used for the analysis (the others were excluded because of lack of data or because stroke was treated by thrombolysis complicated by intracerebral hemorrhage), 32% occurred during warfarin therapy, 27% during aspirin therapy and 42% among those with no antithrombotic therapy. However, only patients in OAC and with an INR >2.0 showed lower incidence of stroke and a lower risk of stroke-related death.33 Stratifying AF patients for risk of thromboembolism is, therefore, crucial. By focusing on the embolic events observed in the control arms of the trials investigating OAC, the Stroke in AF Working Group identified previous stroke/TIA, age, hypertension, diabetes and female gender as predictors of stroke or TIA in AF patients.34 Similarly, the NICE review classified as risk factors for stroke in patients with AF, history of stroke or TIA, age, hypertension and structural heart disease.35 These risk variables have been included in several scores of risk for stroke, as recently reviewed.36 Among these, the CHA2DS2VASc score (Table 1), introduced by Lip et al. in 201037 and “adopted” by the current European guidelines,1 was initially validated in the Euro Heart Survey Cohort. According to this score, the “major” risk factors (age > 75 years, previous stroke/TIA), count for two points, while the other risk factors (systolic heart failure, hypertension, diabetes, age 65–74, vascular disease and female gender), count for 1 point each. With a total score ranging from 0 to 9, low risk is defined when the score is 0, intermediate when it is 1, high risk with a score > 2. The CHA2DS2VASc score has been validated in several cohort studies as being able to better recognize the “truly” low risk and to reduce the number of patients falling in the “intermediate/moderate” interval.36
In a Danish cohort of 73,538 patients with non-valvular AF and no OAC therapy, the rate of thromboembolism was 1.67 (95% CI=1.47-1.89) per 100 patients/year when the “low” risk group was defined by the CHADS2 score and was 0,78/100 patients/year (95% CI=0.58-1.04) when the “low” risk group was identified by the CHA2DS2VASc score. Similarly, the “intermediate risk” group showed a rate of thromboembolism of 4.75/100 patients/year (4.45-5.07) when defined by the CHADS2 score but was 2.01/100 patients/year (1.70-2.36) when identified by the CHA2DS2VASc score. In conclusion, compared to CHADS2, the CHA2DS2VASc score seems to better identify the “high” risk group and to categorize AF patients more accurately.38
The association between AF and stroke is even stronger among older persons. Among 135 individuals with AF enrolled in the Pro.V.A. study, prevalence of stroke was 8.8% as compared to 4.4% among those (n=1441) without AF (p=0.001) while in logistic regression analysis, stroke and AF were associated with an OR of 2.61 (95% CI 1.44-4.70).
Older patients, therefore, could take more advantage with antithrombotic therapy, independently of the presence of other risk factors, as recently suggested by Hobbs et al. who tested different scores of stroke risk. They recorded 54 ischemic strokes, 4 systemic embolisms and 13 TIA among 665 patients aged 75 years and older, with AF and no antithrombotic therapy. All the tested scores demonstrated only a moderate ability to assess the thromboembolic risk, suggesting that all the AF patients age 75 years and older should always be classified at “high risk”, at least until better tools will become available.39
In the past years, thromboprophylaxis in high risk patients relied only on the use of oral anticoagulation by vitamin K antagonists, especially warfarin, which has been demonstrated to prevent strokes better than antiplatelet agents.40 More recently, oral direct thrombin inhibitors (e.g. dabigatran etexilate and AZD0837) and oral factor Xa inhibitors (rivaroxaban, apixaban, edoxaban, betrixaban, YM150) have been tested in clinical practice with several advantages as compared to warfarin. Dabigatran, for example, is non-inferior (when 110 mg bid are used) or even superior (with 150 mg bid) to warfarin in preventing strokes. As compared to vitamin K antagonists, Dabigatran also seems to be safer being associated with lower (lower dose) or with similar (higher dose) rates of major hemorrhages.41 In the AVERROES study, on the other hand, Apixaban has been shown to be superior to aspirin in patients intolerant or not suitable for treatment with warfarin,42 and in the ROCKET AF study,43 rivaroxaban resulted not inferior in preventing strokes as compared to warfarin. These new agents, although not yet fully entered in the common clinical practice, are very promising and will probably modify in the next future strategies for preventing AF-related strokes.
Table 1. Annual risk of stroke predicted by CHA2DS2VASc score (age > 75 years and previous stroke/TIA = 2 points each, systolic heart failure, hypertension, diabetes, age 65–74, vascular disease and female gender= 1 point)
| CHA2DS2VASc score |
Stroke rate (%/year) |
| 0 |
0 |
| 1 |
1,3 |
| 2 |
2,2 |
| 3 |
3,2 |
| 4 |
4,0 |
| 5 |
6,7 |
| 6 |
9,8 |
| 7 |
9,6 |
| 8 |
6,7 |
| 9 |
15,2 |
Atrial Fibrillation and Mortality
As already mentioned, AF is associated with higher risk of mortality because of the strong association both with stroke and HF. AF and HF are related to mortality especially when AF occurs after HF, since AF may represent a marker of more severe HF. Stroke is associated with AF through the altered thromboembolic risk profile of the AF patient. Ischemic strokes are more severe if AF is also present and only prior OAC therapy can reduce ischemic stroke-related mortality in AF patients.
As reported in the European guidelines for AF management, death rates are almost doubled by AF, independently of the presence of other known predictors of mortality.1 Several cohort studies have analyzed this effect of AF on mortality. In the Framingham cohort (more than 5,000 patients followed for 40 years), the presence of AF increased the relative risk of mortality by 50% in men (OR=1.5, % CI 1.2-1.8) and by 90% in women (OR=1.9, % CI 1.5-2.2). This association was also confirmed after the exclusion both of 30-day mortality, where AF could play the role of a “simple” marker of terminal illness, and of patients with structural heart disease at baseline.44 The Renfrew/Paisley study, where 15,406 patients aged 28-64 years were followed for 20 years, showed that AF was an independent predictor of all-cause mortality with a RR of 2,2 ( 95% CI: 1.5–3.2) in women and of 1.5 (95% CI: 1.2–2.2) in men. When only “lone” AF was considered, however, AF was not statistically associated with a higher risk of cardiovascular events or death, although the number of patients with this condition was very small (n=15) .45
Mortality appears to increase especially in older patients with AF. In the Pro.V.A. study, AF was clearly associated with an increase in all-cause mortality after 4 years of follow-up. Among the 135 patients with AF, 59 deaths were recorded (43.7%, mortality rate 128/1,000 person-years), a very high rate when compared to the 280 deaths among the 1,441 patients without AF (19%, 47 deaths per 1,000 person-years). In Cox regression analysis, AF was an independent risk factor for mortality, with a relative risk of mortality, after adjustment for confounders, of 1.47 (95% CI 1.08-1.99).5
Recently, Jabre et al. reviewed the literature and meta-analyzed data from studies looking at the relationship between AF and mortality in patients with myocardial infarction (MI).46 The authors also analyzed the influence of new onset AF on mortality in patients hospitalized for a myocardial infarction (MI) in the Olmsted County–Minnesota cohort, since previous studies were not concordant in attributing an independent effect of AF on hospital mortality. Among the 3,220 patients hospitalized because of MI between 1983 and 2007, 304 had a history of AF, 729 had a first-documented episode of AF post-MI, while 2,187 did not show AF. Among the subjects with new onset AF, the arrhythmia was detected in 218 (30%) patients at the time of the acute MI or within 2 days, in 119 (16%) between 3 and 30 days after MI, and in 392 (54%) thereafter. The analysis revealed that a newly diagnosed AF in the setting of MI was associated with a larger increase in overall mortality with an HR of 3.77 (95% CI, 3.37-4.21). This relation was stronger when AF occurred later, with a 5-fold increase in the risk of death, independently from age, sex, co-morbidities and subsequent HF development.47
AF is the most common arrhythmia in the western world, is an independent risk factor for stroke and is associated with severity of heart failure and with increased all-cause mortality risk. AF prevalence increases with age and, therefore, represents a “growing epidemic” especially in the elderly, with important social and economic consequences. Despite an increasing focus on prevention of cardio-embolic events in recent years, the rising prevalence and incidence of AF and its impact on disability and mortality underline the importance of effective medical management of AF to reduce negative functional and socio-economic consequences.
No disclosures relevant to this article were made by the authors.