Better Lesion Creation And Assessment During Catheter Ablation
Saurabh Kumar, MBBS, PhD, Chirag R. Barbhaiya, MD, Samuel Balindger, MD, Roy M. John MD, PhD, Laurence M. Epstein, MD, Bruce A. Koplan, MD, Usha B. Tedrow, MD, William G. Stevenson, MD, Gregory F. Michaud, MD
Cardiovascular Division, Brigham and Women’s Hospital, 75 Francis St, Boston, MA, 02115.
Permanent destruction of abnormal cardiac tissue responsible for cardiac arrhythmogenesis whilst avoiding collateral tissue injury forms the cornerstone of catheter ablation therapy. As the acceptance and performance of catheter ablation increases worldwide, limitations in current technology are becoming increasingly apparent in the treatment of complex arrhythmias such as atrial fibrillation. This review will discuss the role of new technologies aimed to improve lesion formation with the ultimate goal of improving arrhythmia-free survival of patients undergoing catheter ablation of atrial arrhythmias.
Key Words : Atrial Fibrillation, Contact Force Sensing, Ablation Biophysics, Novel Technologies.
Correspondence to: Dr.Gregory F. Michaud, MD, Cardiovascular Division, Brigham and Women’s Hospital, 75 Francis St, Boston, MA, 02115.
Catheter ablation forms an essential part of the management of cardiac arrhythmias including supraventricular tachycardia (SVT), atrial flutter (AFL), atrial fibrillation (AF) and ventricular tachycardia (VT).1-4 Catheter ablation has demonstrable superiority over anti-arrhythmic drugs in improving arrhythmia burden and quality of life in patients with atrial arrhythmias and SVT.5-12 When the arrhythmia has a well-defined electrophysiologic mechanism and the target region is localized such as in SVT or typical AFL, arrhythmia-free survival approaching 90 to 95% can be achieved.13 However with more complex arrhythmia mechanisms such as AF, arrhythmia recurrence is observed in 50-70% of patients.14,15 This lower efficacy is likely due to limitations in mapping, incomplete understanding of the driving mechanisms of arrhythmia (as is the case in persistent AF), and perhaps most importantly, our inability to create transmural and durable lesions in a linear fashion.
Successful catheter ablation requires not only precise localization of the arrhythmogenic substrate but complete and permanent elimination of that substrate without producing collateral injury. Despite over 30 years of intensive research focusing on novel energy sources, the reliable creation of effective and permanent lesions remains challenging. This review will examine the role of existing and emerging technologies in catheter ablation designed to improve lesion quality during catheter ablation of AF. First, however, it is important to revisit some key concepts in ablation biophysics, which help to define the barriers to better lesion creation, and to explore current methods of assessing an effective lesion.
Radiofrequency (RF) current is the most common and widely employed source used energy source in catheter-based ablation, mainly due to a well-understood safety profile. RF ablation transfers electromagnetic energy into thermal energy by a process called resistive heating at the surface of tissue. Lethal heating destroys deeper tissue by conduction. The RF current is delivered in unipolar fashion between the catheter tip and the indifferent electrode patch placed on skin. In bipolar RF systems, the current flows between two closely apposed small electrodes.
Some important concepts of RF ablation are worthy of review. First, a rise of tissue temperature to above 50°C is required to produce irreversible thermal injury.16-19 and loss of cellular depolarization; with lower tissue temperatures (eg 45-50°C), there may be reversible loss of cellular excitability19 Second, lesion size is proportional to the electrode-tissue interface temperature with higher temperature at the source resulting in deeper heating.19 Third, increasing current flow through the tissue increases resistive heating and thereby lesion size. This third fact is relevant for RF systems that are limited by
calculated power (Watts). Because power = current2 x resistance,
the lower the resistance the greater the current must be to achieve
the same power. One consequence is that the size of the dispersive
electrode has an impact. Increasing electrode surface area leads to
lower impedance through an ablation circuit, resulting in higher
current delivery for a specified power, increased tissue temperature
and thus deeper conductive tissue heating. The addition of a second
dispersive electrode or optimizing skin preparation between the
dispersive electrode and the skin can thereby improve energy delivery
when the system impedance is <100Ω.19,20 Fourth, tissue temperature
decreases predictably with increasing distance from the temperature
source.21 Approximately 90% of the power delivered to the tissue is
absorbed within the first 1-1.5 mm from the electrode surface, hence
only a narrow rim of tissue in close contact with the catheter (2-3
mm)experiences resistive heating. Fixed level energy application
results in a mono-exponential increase in electrode-tissue interface
temperature within 7-10 seconds.22 A thermal gradient of conduction
created in which the tissue further from the ablation electrode may
not reach its stable maximum (thermal equilibrium) until up to 2
minutes later.22 Because of this thermal decay, small increases in
distance from the ablation target may result in large increases in RF
current requirements. Larger current delivery will result in deeper
heating of the tissue layers passively through conduction of a hotter
surface temperature.
Fifth, lesion size is also directly proportional to the radius of the
heat source. Larger electrode diameter (i.e. with larger tip electrodes),
length and contact area all result in a larger source radius and larger
lesion size for the same current density, which is maintained by
increasing power settings when a larger electrode is used.23 It is important to note that lesion size is proportional to electrode-tissue
interface temperature in conventional ablation catheters. With cooled
tip catheters it is proportional to power delivered.
Although heat transfer into tissue should be a predictable biophysical
phenomenon, in vivo, other factors (including the cooling effect of
regional blood flow, and blood flow through the tissue) alter the heat
transfer to tissue, making it less predictable. Once tissue temperature
reaches or exceeds 70°C, coagulum can form at the electrode tissue
interface and a sudden rise in electrical impedance can occur, that
limits energy delivery. There is evidence that protein denaturation
may start at temperatures around 55°C,22 which is probably the first
step in the cascade that leads to coagulation formation. Reaching
temperatures of 100°C also can results in “steam pops”, that may
lead to perforation and cardiac tamponade.24 Convective cooling is a
major thermodynamic factor opposing the transfer of thermal energy
to deeper tissue layers by limiting surface temperature, however it
is exploited because cooling the catheter tip allows greater energy
delivery without boiling or coagulum formation at the electrode tip;
thus, increasing the amount of current that produces direct resistive
heating increases the radius of the effective heat source. For these
reasons, greater depth and increased diameter of lesions can be
produced with cooled-tip catheters.24 Electrode tip cooling can be
achieved passively with large tip ablation electrode or actively with
closed or open-tip irrigated catheters. Electrode tip cooling, however
limits the value of temperature monitoring during irrigated catheter
ablation, as there is a larger disparity between electrode and tissue
temperature.19
Factors that influence passive cooling at the electrode-tissue
interface include the magnitude of regional blood flow and stability
of the electrode catheter on the tissue surface.25 The tricuspid and
mitral valve annuli have high volume of regional blood flow. When
endocardium is smooth, catheter stability may be difficult. Both
of these factors can decrease lesion size. In contrast, ablation in
trabeculated myocardium or under valve leaflets can result in highly
efficient heat transfer and risk of excessive tissue heating. Other
factors such as electrode-tissue contact force (CF) can directly affects
lesion size, depth and volume and this will be reviewed in detail
in subsequent sections.20 Because of the variability of these factors
in vivo, applied energy, power and current are poor indicators of
the extent of lesion formation during RF ablation.19,20,22 However,
as tissue is heated, there is a temperature-dependent fall in tissue
impedance.26 that is a useful surrogate for lesion formation. The
availability of contact force measurements has also improved the
ability to create reliable lesion size.
In summary there are multiple factors that effect RF ablation
lesion size including power, ablation electrode temperature, duration
of energy delivery, ablation circuit impedance, catheter-tissue CF,
electrode size and myocardial blood flow. It is important to note
that although larger RF ablation lesions can increase the success of
ablation, they can also increase the risk of collateral tissue injury, for
example, to the esophagus during pulmonary vein isolation (PVI).
It is thus critical to revisit our motivation for attempting to create
larger, more permanent RF lesions.
The Need For Better Lesion Creation
It is now well accepted that the pulmonary veins (PVs) play
a critical role in the initiation and maintenance of AF.27 and that
complete electrical disconnection of the PVs from the left atrium (LA) is an important electrophysiological endpoint.28-30 Although
electrical disconnection can be achieved almost universally by the
end of the procedure, long term efficacy of catheter ablation remains
soberingly modest, with single and multiple procedure success rates
of 54% and 79% recently reported for paroxysmal AF over long
term follow up (≥ 3 years).14 The time-dependent inevitability of
PV reconnection and its relationship to future AF recurrence has
been demonstrated in many studies showing that, prior to the
use of contact force for guiding ablation lesions, up to 50-64% of
PVs reconnect during an intra-procedural waiting period of up to
60 minutes post acute PV isolation.31-33 It is well appreciated that
AF recurrence post catheter ablation is usually associated with
resumption of PV-LA conduction.28,29,34 Gaps in lines that allow
PV to LA reconnection allow PV triggers to also serves as a triggers
for other macro-reentrant atrial arrhythmias and as the substrate for
some macroreentrant atrial tachycardias after circumferential antral
PVI.28,29,31,34,35 In a histopathologic study in patients undergoing
MAZE for recurrent AF after initially successful catheter ablation
for AF, Kowalski et al performed intraoperative assessment of PV-LA
junction conduction during the procedure and took biopsies from the
PV antrum at sites of endocardial scar. They found that PVs showing
electrical reconnection after catheter-based RF ablation frequently
exhibited either anatomic gaps or non-transmural lesions at sites of
ablation. However, non-transmural lesions in some PVs had evidence
of persistent PV-LA block suggesting that fact that lesion geometry
may influence PV conduction.36 Indeed, gap geometry plays a critical
influence on conduction through discontinuities in RF lesions such
that bifurcated (“Y” shaped) or angled gaps (containing two right
angles within the conduction path) were less likely to produce
bidirectional conduction block but were more likely to produce
unidirectional or rate dependent conduction block compared with
straight gaps.37
Ineffective lesion formation is the hallmark of PV-LA conduction
recovery and recurrence of arrhythmia. Despite an apparently successful lesion, conduction recovery may occur. At such a site, there
may be acute loss of electrical signals and electrical inexcitability
as both reversible and irreversible cell injury have occurred, and
in fact, acute PVI may be achieved by a combination of reversible
and irreversible circumferential tissue injury.38 A broad anterograde
wavefront of edema on the leading edge of each lesion may be present
that is capable of producing conduction block. This possibility may
explain why PVI can often be achieved without complete PV
encirclement.39 With time, tissue at the boundary of the lesion
recovers normal conduction over the course of 1-4 weeks.40 This
allows gaps within an ablation line or boundary to remain undetected
(i.e. electrically silent) during the index procedure. With time as tissue
recovers, conduction occurs through gaps in the ablation lines.41
Aside from deficiencies in mapping and imprecise understanding
of arrhythmia mechanism, it is clear that a permanent and effective
energy source with efficient tissue specificity to permanently
eliminate arrhythmogenic substrate, yet avoiding unnecessary
collateral damage is of paramount importance in the goal to improve
ablation efficacy and long term arrhythmia-free survival in patients
with AF. These methods must be combined however, with means for acutely assessing creation of an effective lesion.
How Effectively Do We Identify A “Better” Lesion?
As discussed previously, RF ablation produces thermal injury.
Permanent myocardial necrosis requires that a tissue temperature
beyond 50° C is achieved.16-19 However, tissue temperature is not
measurable in patients and is not indicated by the intraelectrode
temperature measurement provided by irrigated RF ablation catheter
electrodes.
There are a limited number of intra-procedural methods for
assessing completeness. Impedance at baseline and subsequent
changes during ablation have been used as surrogates for cathetertissue
contact and for predicting lesion efficacy in a number of
experimental studies.42-47 Higher impedance with greater electrodetissue
contact is thought to be due to larger interface area between
the electrode and tissue. In contrast, lower impedance recorded
with lower electrode-issue contact is due to lower resistivity of
blood compared to myocardium and greater interface area between
the electrode and blood. However, impedance varies at different sites in the heart, and the baseline impedance does not appear to
be a reliable indicator of RF ablation lesion creation.48,49 With RF
application, tissue heating results in reduced myocardial resistivity
and a fall in tissue impedance.44,46,47 Animal studies have shown that
the magnitude of impedance fall early after the onset of RF ablation
strongly correlates with lesion depth (correlation co-efficient squared,
R2 = 0.6845), diameter (R2=0.6645) and/or volume (R=0.7242-45,47). Furthermore, CF influences the rate and duration of
impedance decrease with “poor” contact lesions resulting in earlier
plateau (≤13 seconds) compared to “good” contact during which a
continuous fall in impedance may reach a later plateau (eg plateau at
40 seconds).45
In human studies, the extent of fall in impedance has been shown to
correlate with the CF.48,50 Kumar et al. showed that there was modest
linear relationship between CF during ablation and the impedance
fall (r=0.32, P<0.001). Similarly, de Bortoli et al. found a stronger
association between contact force and maximum impedance fall (r= 0.54, P<0.01).50 An impedance fall of 10 ohms at 10 seconds was
shown to correspond to a contact force < 20g. However there was a
large degree of overlap between different ranges of CF and impedance
fall was only able to roughly differentiate low, intermediate and high
CF beyond 15 seconds of RF (Figure 1).48
Figure 1. Relationship between maximal impedance fall and average CF or FTI. Definitions of low, intermediate and high CF were ≤20 g, 21–60 g and >60g respectively and for FTI were (≤500 g*s), 501–1000 g*s and >1000 g*s, respectively. There was a moderate correlation between maximal impedance fall, average CF (A) and FTI (B) during ablation. Note, however that there is a wide variation in CF or FTI( vertical scatter of dots) at any 1 particular impedance fall value. Maximal impedance fall was significantly greater with each increment in CF category (C) or FTI category (D). Note, however that there is a large degree of overlap in the magnitude of impedance fall between different CF or FTI categories. From Kumar et al48 permissions obtained

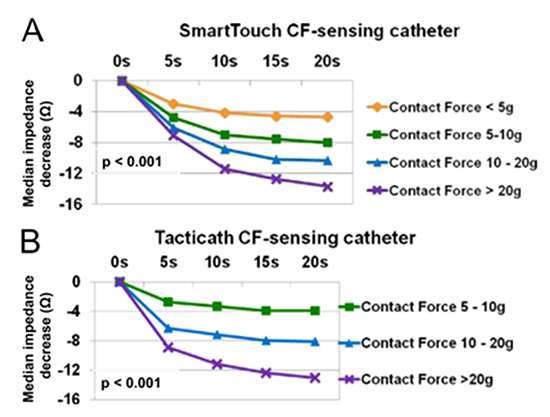
These findings were confirmed by an independent study by
Reichlin and colleagues.51 In that study, the impedance decrease in
the first 20 seconds was larger with increasing average category of
CF over the same time. CF <5 g, 5-10 g, 10-20 g, and <20 g was
associated with a median fall in impedance at 20 seconds of 5 ohm
(interquartile range [IQR].2-7 8 ohm.4-11 10 ohm.7-16 and 14 ohm.10-19
with one commercially available CF sensing catheter (SmartTouch,
Biosense-Webster, Diamond Bar, CA, USA). Similar findings have
been noted with another type of CF-sensing catheter (Tacticath, St.Jude Medical, St. Paul, MN, USA) (Figure 2).51,52 A major limitation
of impedance monitoring is that it is useful only after ablation has
begun. Furthermore, the relationship between impedance fall and
lesion formation is imperfect. It is controversial whether impedance
drop give reliable information about lesion formation. Many factors
such as body surface characteristics (e.g. chest), indifferent electrode
position, and hemodynamic conditions, make the correlation between
impedance and CF imperfect.53 In addition, there is no fixed value of
impedance drop that has shown to reliably predict transmural lesion
formation.
Figure 2. Initial impedance decrease (within the first 20 seconds) is greater with higher average CF. Shown are the median values of absolute impedance decreases in ohms (Ω) within the first 5, 10, 15, and 20 seconds during RF performed with the SmartTouch CF-sensing catheter (A) and the TactiCath CF-sensing catheter (B) according to the achieved CF for the groups o5g, 5–10 g, 10–20 g, and >20 g. Adapted from Reichlin et al,51 permissions obtained.
The effectiveness of a lesion also may be assessed from a change in
electrogram (EGM) amplitude or morphology or increase in pacing
threshold at the site54,55 EGM changes have been described as a
surrogate for lesion transmurality. A reduction in EGM amplitude
of <80% is thought to indicate a transmural lesion.56 Changes in
unipolar and bipolar EGM morphology post versus pre- ablation
may also detect lesion transmurality.57 Elimination of the negative
deflection on the unipolar EGM identified a transmural lesion
with 100% sensitivity and specificity in an animal study.57 Indeed,
continuing RF application until the creation of a completely positive
unipolar signal at a particular site was associated with improved AFfree
survival compared to empiric 30 seconds of RF at each site alone
during PVI in one non-randomized study.58 It is important to note
that unipolar distal EGM amplitude changes are likely to provide
more useful information than bipolar recordings as the signal from
the ring electrode may dominate the EGM bipolar amplitude and
wavefront of activation is less important.22
Although changes in EGM properties have been used to guide
lesion effectiveness, the magnitude of change in pacing threshold
with RF ablation has been shown to be substantially greater than the
magnitude of decrease in bipolar or unipolar EGM. In the atrium,
loss of bipolar capture post ablation predicts formation of a uniform
transmural lesions.59 and is superior to EGM-based detection of gaps
within ablation lines.60,61 In the ventricle, change in pacing threshold
correlates with and is a better marker of lesion size than change in
unipolar or bipolar EGM amplitude.54 In human studies, RF ablation
with the endpoint of electrical inexcitability along a circumferential
line during a PVI has been shown to markedly enhance single
procedure success of AF ablation compared with the aim of achieving
bidirectional PV-LA conduction block alone.61 It may also reduce
acute PV reconnection rates and dormant conduction.62
Real-time MRI, and MRI thermography, although not readily
available, are promising methods for intra-procedural assessment of
lesion completeness.41,63,64 Cardiac MR imaging appears capable of
delineating areas of permanent tissue damage caused by ablation, and
of identifying gaps in atrial ablation lesion lines in animal studies.41,63
Important limitations exist when using methods to define a
“better lesion”. The gold standard of transmural tissue necrosis
by histopathology is highly relevant for animal models, but is not
applicable clinically. Thus the effectiveness of any new technology in
human studies is primarily assessed by acute and long term clinical
outcomes, which are clearly the most clinically relevant goals. Further
work is thus needed to validate simple intra-procedural parameters
for assessing acute lesion efficacy that reliably translate to long-term
procedural success.
Technologies For Better Lesion Creation
There has been a rapid expansion of research aimed at improving the efficacy, simplicity and speed of catheter ablation. A number
of “single shot” devices such as endoscopic ablation systems,
multielectrode catheters, and balloons seek to provide a simpler and
quicker approach to PVI. Whether these technologies will be more
effective than traditional point-by-point RF ablation has not been
established, and has been reviewed elsewhere.65-67 In this review we
will discuss: (i) improvement in our ability to assess real-time catheter
tissue contact with force sensing; (ii) variation of existing systems
that allow creation of deep intramural lesions (bipolar ablation); (iii)
catheters that allow extensive and deep myocardial lesions without
significant damage to collateral structures (electroporation).
Two new contact force (CF) sensing catheters are now available for
clinical use in the USA: the TactiCath (St. Jude Medical, St. Paul, MN,
USA) and SmartTouch Thermocool (Biosense Webster, Diamond
Bar, CA, USA) catheters. These allow real-time measurement of the
catheter tip-to-tissue CF during catheter ablation.43,68-72
Tacticath is a 7 French (Fr) open irrigation catheter (6 holes
at the distal tip) with a 3.5-mm tip electrode, and a force sensor
incorporated into the distal part of the catheter between the second
and third electrode. The force sensor has a deformable body (elastic
polymer) and 3 optical fibers that measure micro-deformations
correlating with force applied to the catheter tip. Infrared laser light is
emitted through the proximal end of the 3 optical fibers. The light is
reflected by fiber Bragg gratings on the deformable body at the distal
end of the optical fibers, near the tip of the catheter. Applying CF
to the tip of the catheter produces a microdeformation, causing the fiber Bragg gratings to either stretch or compress, thereby changing
the wavelength of the reflected light. The change of wavelength
is proportional to the CF applied to the tip. The system is able to
calculate and display the vector of the CF (magnitude and angle)
at a sampling rate of 100 milliseconds (ms). It has a resolution and
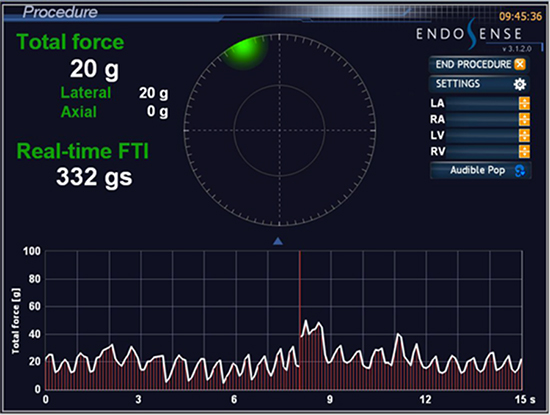
sensitivity of about 1 gram in bench testing.43,70 During RF delivery,
the force–time integral (FTI; measured in grams x seconds, g*s) is
displayed (Figure 3).
Figure 3. Tacticath CF-sensing display (From Wong et al,77 permission obtained).
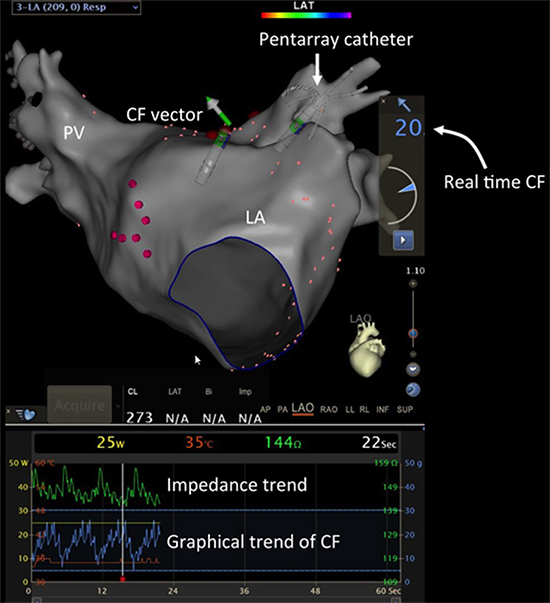
The SmartTouch Thermocool catheter is a steerable, 3.5-mm sixhole
open-irrigated tip ablation catheter. The catheter tip electrode
is mounted on a precision spring that permits a small amount of
electrode deflection. A transmitter coil that is coupled to the tip
electrode, distal to the spring, emits a location reference signal.
Location sensor coils placed at the proximal end of the spring detect
micromovement of the dRecently, there has been renewed interest
in this technology and a novel irreversible electroporation (IRE)
modality that can ablate myocardial tissue using DC energy level
lower than the arcing threshold has been developed. IRE is capable
of creating large myocardial lesions and interestingly, there seems to be a greater safety margin for achieving large myocardial lesions
without damage to surrounding structures such as the epicardial
coronary arteries. The impetus for this interest is derived from the
fact that RF ablation near coronary arteries can lead to acute vessel
injury, and also progressive vessel stenosis from tunica intima and
media thickening.117-120 Tissue cooling by arterial flow can also
lead ineffective lesion formation and unsuccessful ablation at sites
adjacent to an arterial branch.121
Figure 4. SmartTouch platform with the CARTO mapping system (Biosense Webster)
In pre-clinical work IRE catheters (7 French).115,122-127 have been developed in varying shapes (circular, linear) and varying number of
electrodes.8-10 Energy is applied between the electrodes and a remote
indifferent electrode using a monophasic external defibrillator
charged to delivery energy in a range of 50 and 360 J.122 In animal
work, greater applied current through IRE resulted in a linear
increase in median lesion depth. No signs of thermal damage to
the electrode or ablation site (when examined histologically) were
seen, suggesting that the putative mechanism of injury is likely nonthermal,115 though tissue temperature was not examined specifically
in those studies. Furthermore the region of IRE-induced injury did
not have a sharp “cut off ” as is usually seen grossly with RF lesions ,
but often irregular borders were observed.115
IRE, when used to deliver a single pulse, non-arching 200J
application between the catheter and an indifferent electrode patch at the PV ostia of swine (maximum 4 pulses/pig), resulted in acute PV
EGM attenuation, increased PV stimulation threshold, and no PV
stenosis with a 3.5 mm-deep lesions histologically at 3 weeks’ follow
up.127 In a follow up study in pigs, IRE to PVs resulted in acute PV
stenosis that reversed at 3 months; in comparison, RF application
at equivalent sites resulted in acute PV stenosis that persisted at 3
months.126 Epicardial IRE in pigs, caused extensive myocardial
lesions whilst preserving coronary artery patency and wall integrity.122
Lesion depth and width increased with energy of electroporation
applications in swine epicardium with reproducible transmurality
observed and, critically, no evidence of intimal hyperplasia of
the coronary arteries located within the regions of myocardial
damage.123,124 Further studies in pigs have shown epicardial IRE
delivered intentionally overlying major epicardial coronaries resulted
in short-lasting (<30 minutes) luminal narrowing in the targeted
area with subsequent normalization, suggesting coronary spasm.125
No injury to organs adjacent to the pericardium was noted.123
Importantly, there was myocardial injury to tissue surrounding the
arteries, as the presumed mechanism of injury was not related to
tissue heating. This finding is of particular interest as myocardial
sparing around an artery is not uncommon in RF or cryoablation as
a result of tissue cooling (or warming) by arterial flow.128,129 Overall,
the findings from the intriguing animal work suggests that the
myocardium may be more sensitive to electroporation injury than
the coronary arteries, a property that could be potentially exploited
in the future in epicardial ablation. However, important issues such
as controlling lesion size (wide ranges of lesion depths were noted in
some studies), effect on phrenic nerve injury, the prevention of acute
coronary artery vasospasm, and long term effects on the coronary
lumen are important issues that need to be addressed116 The catheter
has not been tested in humans and is not available for use in the
USA. It is likely to have important clinical applications if safety and
efficacy can be demonstrated.
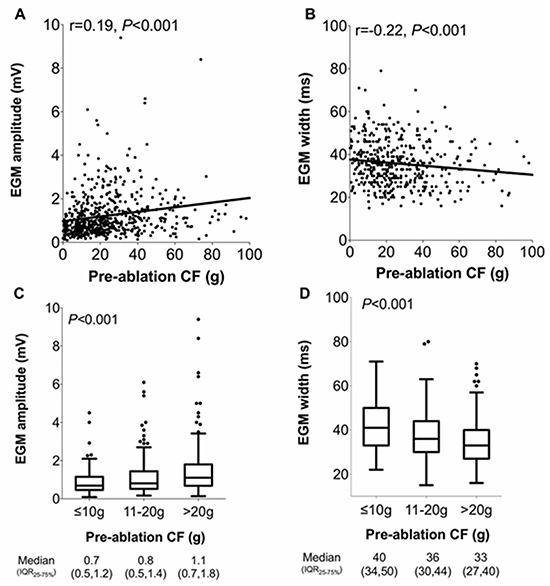
Figure 5. Graphs showing that pre-ablation CF and EGM characteristics such as EGM amplitude and width (A,B) had a modest positive and modest negative correlation respectively with increasing preablation CF; median EGM amplitude increased (C) and median EGM width decreased (D) with increasing pre-ablation CF category but note the large degree of overlap in values with different CF categories. Adapted from Kumar et al,83 permission obtained.
Other Technologies For Assessing RF Lesion Creation
A number of other technologies have been tested that will be
mentioned briefly. None are available for clinical use at this stage.
Direct endocardial visualization (IRISTM Ablation Catheter,
Voyage Medical, Redwood City, CA, USA) are catheters that allow
direct visualization of tissue characteristics (for example dense scar
versus border zone in infarcted ventricles), to monitor catheter
location and stability, lesion development and lesion contiguity.130,131
In one study, this catheter created wider lesions at lower power
compared to irrigated tip ablation but with comparable pacing and
sensing efficacy.131 In an animal model, visually-guided RF ablation
in the ventricle resulted in more reliable lesion creation as assessed
on histopathology compared with standard open irrigated catheter
guided by “traditional” markers of contact where only 78% of lesions
delivered were identifiable histologically.132 This technology appears
promising in improving the efficacy of ablation using currently
available RF-methods.
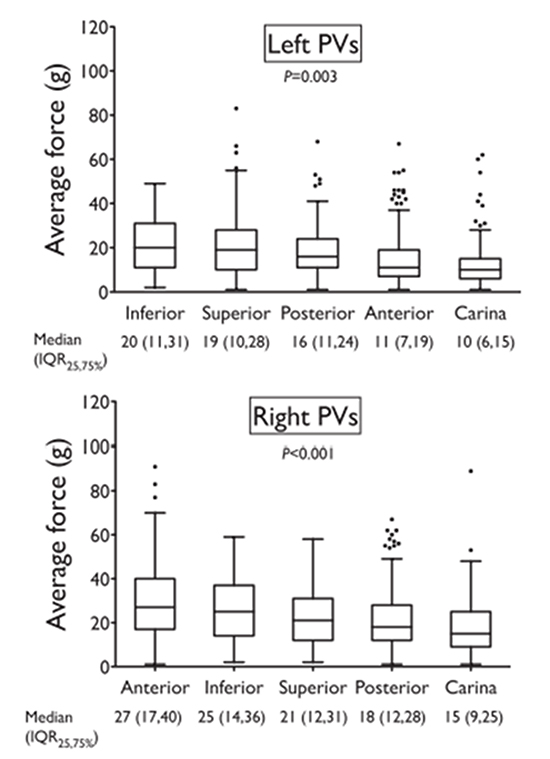
Figure 6. Range of CFs obtained during PVI performed by experienced operators using conventional methods of contact include EGM amplitude, tactile feedback, catheter motion on fluoroscopy and the mapping system and impedance fall. Operators were blinded to real-time CF readings. Note the wide variation in CF readings within each PV segment. For example at the left superior PV segment, the CF varied from 0-80 g. Also note that the lowest CFs was at the carina and anterior PV segment on the left and the carina of the right PVs. From Kumar et al,87 permissions obtained.
Investigators have previously demonstrated that variable catheter
tip sliding can lead to poor tissue contact, compromise lesion efficacy
and create unpredictable lesion dimensions.79 Electrogram-gated
pulsed RF ablation is a variation of currently available RF technology
that aims to deliver the same average power as a conventional ablation
but for a shorter duration based on the onset of the local electrogram.
This method aims to counteracts the effects of sliding catheter
movement that results in degradation of ablation efficiency. This
system was shown to create consistently deeper lesions irrespective
of the degree of catheter movement as well as reaching target lesion
depths significantly faster than conventional ablation in one study
carried out on a thermochromic gel myocardial phantom. Further
work is needed to validate this technology in vivo.25
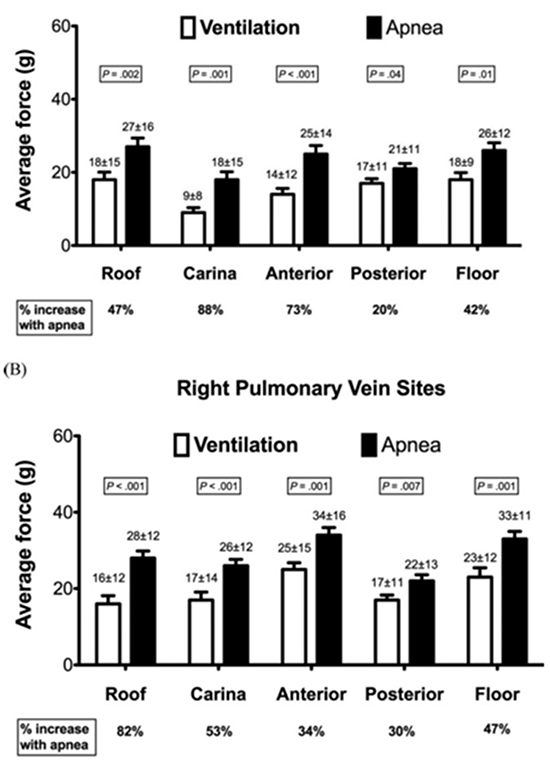
Figure 7. Average CF is significantly higher during short RF ablation performed with short duration apnea compared with ventilation. From Kumar et al,89 permissions obtained.
Acoustic radiation force impulse (ARFI) imaging is an ultrasoundbased
technique that allows quantification of tissue stiffness based on
mechanical displacement of tissue in response to ultrasonic impulses
and monitors the tissue response using conventional ultrasound
methods. The technology can be utilized with intracardiac echo
(ICE) and can visualize the relative elasticity difference between
ablated and unablated myocardium and can accurately assess focal
RFA lesion morphology in vitro.133,134 This technology has the
potential for guiding lesion transmurality in the future.
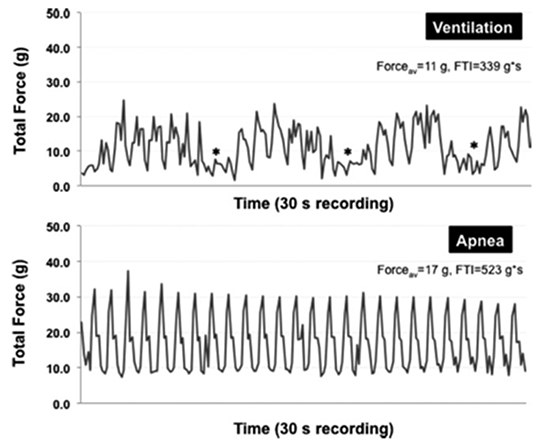
Figure 8. Real-time recordings of CF during ventilation compared with apnea at 2 anatomically adjacent sites on the cavotricuspid isthmus. With ventilation, there is an abrupt drop in contact force with each respiratory swing (marked with asterisk), which is absent during apnea. Swing in CF during cardiac motion is similar (~15 g). Adapted from Kumar et al,89 permissions obtained.
A number of important developments have been made in catheter
ablation aiming to improve lesion creation whilst minimizing
collateral injury and improving long term arrhythmia free survival.
With each new development, one must be wary of potential for
harm not uncovered from small pre-clinical or clinical studies.
Randomized controlled data is valuable in validating and accepting
the superiority of new technology compared to traditional methods
of catheter ablation, but the safety and efficacy of each technology
must be tested in a systematic fashion. Rigorous surveillance of safety
is important to prevent avoidable harm to patients. Progress has
been made, but further work is needed on intra-procedural methods
of identifying lesion completeness that reliably predict arrhythmiafree
survival in long term follow up.
Dr. Kumar is a recipient of the Neil Hamilton Fairley Overseas Research scholarship co-funded by the National Health and Medical Research Council and the National Heart Foundation of Australia; and the Bushell Travelling Fellowship funded by the Royal Australasian College of Physicians. Dr. Tedrow receives consulting fees/honoraria from Boston Scientific Corp. and St. Jude Medical and research funding from Biosense Webster, Inc., and St. Jude Medical. Dr. John receives consulting fees/honoraria from St. Jude Medical. Dr. Epstein receives consulting fees/honoraria from Boston scientific Corp., Medtronic, Inc., and Spectranetics Corp. Dr. Michaud receives consulting fees/honoraria from Boston Scientific Corp., Medtronic, Inc., and St. Jude Medical, and research funding from Boston Scientific Corp., and Biosense Webster, Inc. Dr. William Stevenson is co-holder of a patent for needle ablation that is consigned to Brigham and Women’s Hospital. The remaining authors have no disclosures.