Stroke is a leading cause of morbidity and mortality, killing up to 140,000 people in the United States every year [1]. Up to 90% of strokes are ischemic (vs. hemorrhagic or lacunar) with 15-20% occurring secondary to atrial fibrillation (AF). Compared to patients without AF, thromboembolic strokes due to AF are more likely to be fatal and/or debilitating. Because AF is often asymptomatic, the AF-attributable stroke risk is likely substantially underestimated [2]. Other etiologies of ischemic stroke include aortic and cerebrovascular atherosclerosis and non-AF related thromboembolic disease.
Non-AF risk factors for both stroke as well as atherosclerotic vascular disease include age, hypertension, hyperlipidemia, diabetes mellitus, and genetic predisposition [3]. Notably, many of these same clinical and anatomical factors that contribute to non-AF-related stroke or thromboembolism (TE), also underlie and predict AF as well.
Recently, clinical studies of patients with implanted pacemakers or defibrillators have shown both a substantial incidence of clinically unrecognized AF (e.g. subclinical AF (SCAF)) and an epidemiologically increased risk of both stroke and mortality when SCAF is present in such patients [4] [5]. More recently, clinical trials using inserted cardiac monitors (ICM) in patients without known AF but with demographic and/or laboratory features common to AF, including older age, hypertension, diabetes, and heart failure have shown a high likelihood of such patients having SCAF [6]-[8]. Detection rates have been as high as 40% by 30 months of monitoring [6].
Thus, in an AF patient, is a TE consequent to the AF or consequent to the comorbidity underlying the AF? In parallel, in a patient with cardiovascular disease (CVD) and a TE event, but without known AF, is the event due to the CVD or is it due to as of yet unrecognized but monitor-detectable AF?
Technological advances in medicine have increased not only our ability to treat disease but also to better comprehend its pathophysiology. With these discoveries, classic cause and effect roadmaps may become muddied. AF and TE risk, including stroke, is a good example. We suggest herein the possibility that a subset of patients without known AF but with the presence of CVD may actually have SCAF that contributes to the overall likelihood of TE. In other words, stroke risk that has been associated with elevated CHA2DS2-VASc (congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, stroke or transient ischemic attack, vascular disease, age 65-74 years, gender) scores in the absence of AF [10]-[17] may not always be truly absent AF. Improved patient identification and screening strategies to detect SCAF, and treat accordingly, may reduce associated cardiovascular morbidity in this population.
Although the CHA2DS2-VASc score: (a) is a validated stroke prediction tool in patients with non-valvular AF; (b) is designed to identify AF patients who warrant prophylactic anticoagulation; and (c) is now the major guideline-recommended risk prediction tool in AF patients, having improved upon the original CHADS2 score by refinement of low-intermediate risk AF patients [9]; a myriad of studies have demonstrated the ability of both scores to predict stroke or TE even in the absence of AF. Liu et al. published a meta-analysis and systematic review designed to evaluate the accuracy of CHADS2 and CHA2DS2-VASc scores in non-AF populations. They pooled 6 trials and ultimately demonstrated good sensitivity. However, both scores were subject to inherent heterogeneity and poor specificity, most likely due to failure to consider stroke subtype (e.g. ischemic or hemorrhagic) [10]. A separate large study of nearly 1,800 patients with first ever ischemic strokes without known AF documented the ability of pre-stroke CHADS2 and CHA2DS2-VASc scores to predict stroke recurrence, cardiovascular events, and 5-year mortality [11]. Further, both scores have been associated with stroke risk and other adverse cardiovascular events in non-AF patients with coronary artery disease and/or those undergoing cardiac surgery [12]-[14]. More recently, Nayyar et al. have shown that the risk in non-AF patients with elevated CHA2DS2-VASc scores may be highest if intra-atrial block is also present, which is known to be associated with an increased incidence of AF [15].
The predictive ability of these scores, despite the absence of AF, also appears to span other areas of structural heart disease. Wolsk et al. evaluated >100,000 patients admitted with heart failure in sinus rhythm and confirmed that the CHA2DS2-VASc score could predict TE rates within the first year of follow up, with diabetes, age, vascular disease, and prior TE independently conferring increased risk [16]. Even a retrospective analysis of a small cohort of patients with left ventricular non-compaction demonstrated higher CHADS2 and CHA2DS2-VASc scores in patients with than without stroke or TE [17].
While the relationship between CHA2DS2-VASc score and increased stroke/TE risk may exist because many of the score’s components are independent mechanisms of stroke even in the absence of an intracardiac thrombus, the ICM trials noted above suggest that SCAF is likely present in many such patients, and therefore, that some of the reported stroke/TE events in these CVD patients, unknown to have AF, may in fact be due to SCAF with AF-related thromboembolism [Figure 1] and [Figure 2]. Importantly, in addition to quantifying stroke risk, the CHA2DS2-VASc score also correlates with the development of SCAF, especially when diabetes and/or heart failure are also present [18].
Figure 1. AF and Ischemic Stroke.
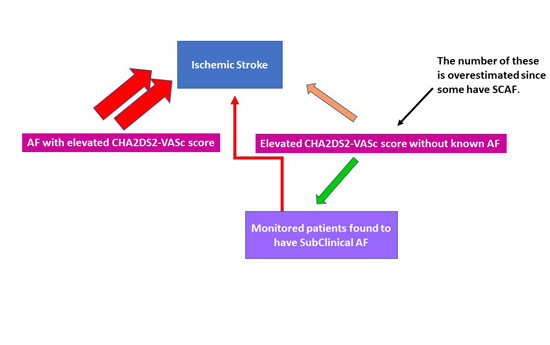
Contributors to ischemic stroke in patients with AF include AF and the associated comorbidities that constitute the CHA2DS2-VASc score. Note, some of those without known AF in fact have subclinical AF (see text).
Figure 2. Major Etiologies of Ischemic Stroke
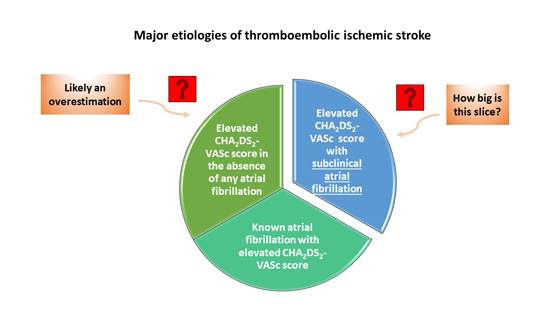
Note: Those without known AF are likely overestimated since some of these must have AF, given our current knowledge about subclinical AF (see text).
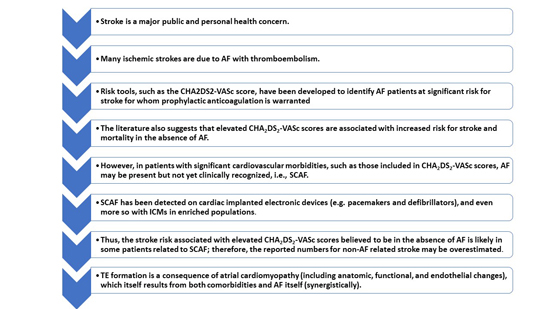
Thus, we suggest herein that some of the TE risk associated with CVD and an elevated CHA2DS2-VASc score may actually be related to SCAF and that the magnitude of risk reported directly consequent to or associated with comorbidities that contribute to elevated CHA2DS2-VASc scores in patients without known AF may overestimate their direct causative relationship. In this context, the true risk of stroke or TE is likely related to the magnitude of synergy between CVD comorbidities and AF and their combined contribution to left atrial thrombus formation [Figure 3].
Figure 3. Concepts regarding ischemic stroke, AF, and concomitant comorbidities.
The concept of “atrial cardiomyopathy” is increasingly evoked as a potential link between atrial arrhythmias and TE. Termed the “common pathological denominator of all forms of AF”, the same predictors included in the CHA2DS2-VASc score are known to cause myopathic changes in the atria [19]. Thus, importantly, left atrial thrombus formation and cardioembolic disease are directly related to the underlying substrate of the left atrium and not solely due to AF alone. This helps to explain why patients with AF but without CVD (e.g. “lone AF”) have comparably lower stroke risk [20] and that TE risk increases as CHA2DS2-VASc score increases. Moreover, there is often temporal discordance between the onset of AF and a TE event [21], again sugesting a role for the underlying atrial myopathy beyond simply the presence of AF. Further it is well understood that restoration of sinus rhythm does not immediately mitigate stroke risk, especially in the early post-cardioversion period [22]. To what extent the presence and type of cardiomyopathy is an independent predictor of stroke and/or to what extent AF leads to atrial remodeling independent of cardiovascular disease or age-related effects is unknown, but it is likely that the processes are occurring both in parallel and in series [23], [24]. Hence, to fully quantify stroke risk, one needs to consider atrial-affecting disorders and timing and burden of AF synergistically [4], [25].
That the number, type, and magnitude of associated disorders as well as AF burden can all relate to stroke risk seems inherent. But, what about the timing between AF and stroke? Why can ischemic strokes be temporally unrelated to the immediacy of AF? For example, in some studies, the last AF event prior to a stroke occurred >30 days before, while in others, such as the CRYSTAL AF study, [26] AF is first demonstrated on continuous monitoring initiated one or more years post stroke. The reasons include the fact that atrial endothelial, metabolic, anatomic, histopathologic, and contractile alterations associated with factors contributory to the atrial cardiomyopathy (as discussed above) can each contribute to the prothrombotic state and may not resolve either immediately or completely upon cessation of AF (whether paroxysmal AF, cardioverted AF, or SCAF) [21]. Thus, neither may the prothrombotic state. Moreover, if a clot forms during a period of AF, it need not embolize synchronously with the termination of AF. Conceptually, it may even be more likely to do so after some improvement of atrial contractile function following AF cessation. Thus, AF may contribute to causation but not be present at the time of thromboembolism [21]. Additionally, beyond a diseased left atrium, cardioembolic stroke can also arise from a patent foramen ovale, myopathic left ventricle, atrial myxoma or other vascular etiologies, independent of AF [27].
Not surprisingly, increasing duration of SCAF as well as comorbidity severity correlates with increasing stroke risk [8], [28]-[31]. Accordingly, since SCAF-associated thromboembolic risk depends not only upon AF burden but also on the type and severity of associated comorbidities, longer AF durations may result in stroke when comorbidities are less severe while lower AF burdens may result in stroke only when more severe comorbidities are present as has been clearly demonstrated by both Botto et al. [30] and by Kaplan et al. [31] The key is the presence and degree of left atrial cardiomyopathy either or both may synergistically-create.