Recurrent Takotsubo Cardiomyopathy During Cryoablation Procedure for Atrial Fibrillation: A Case Report
Nadeem Khan1, Alejandro Jimenez Restrepo2, Sanjay Kumar3
1Department of Medicine, Marshfield Clinic, Wisconsin.2Division of Cardiology, Marshfield Clinic, Wisconsin.3Division of Cardiology, Marshfied Clinic, Wisconsin.
We report a case of 72-year-old female with prior history of takotsubo cardiomyopathy (TSC) who had recurrence of TSC during cryoablation of pulmonary veins for atrial fibrillation (AF) ablation. This case is unique because this is the first report of TSC detected during cryoablation and the procedure being stressor for recurrent TSC. We discuss possible mechanism of TSC and management of this case. Readers would have higher alertness of detecting TSC during AF ablation and therefore would be able to manage this serious condition properly.
Key Words : Atrial fibrillation, Ablation, Takotsubo cardiomyopathy, Cryoablation, Recurrent takotsubo cardiomyopathy.
Sanjay Kumar, M.D., F.A.C.C.
Division of Cardiology
3501 Cranberry Blvd
Weston, WI 54476
We present a case of a 72-year-old Caucasian female with a previous history of hypertension, coronary artery disease, resolved takotsubo cardiomyopathy (TSC) and symptomatic paroxysmal atrial fibrillation (AF), who underwent cryoablation of pulmonary veins (PV) for AF. She developed recurrent TSC following cryoablation of left inferior pulmonary vein. Intense vagal response to cryoablation was followed by epinephrine injection to restore circulation. Epinephrine injection or possible ganglionic plexus response could be implicated as trigger for TSC recurrence. This reports increases awareness of ganglionic plexus (GP) response and management considerations associated with cryoablation of pulmonary veins for AF.
A 72-year Caucasian female with history of stable coronary artery disease, right coronary artery stenting for abnormal stress test and preserved ejection fraction (EF) had episode of cervical discitis in year 2011. She had fever and neck stiffness which resolved with antibiotic therapy. During this episode she had chest pain and electrocardiogram (EKG) showing anterior T wave inversions. Her left ventricular (LV) ejection fraction (EF) was 45% (previously 65%). The entire apex was severely hypokinetic to akinetic. She had coronary angiogram, which revealed mild diffuse stenosis of all three coronary vessels with patent stent in the right coronary artery. Apical wall motion extended beyond one coronary artery territory, a typical finding for TSC. Repeat echocardiogram after 5 weeks showed resolution of apical wall motion abnormality and normalization of EF confirming diagnosis of TSC.
In July 2012, she started noticing palpitations and dyspnea. An event monitor was placed, which revealed paroxysmal AF. She was started on warfarin, amiodarone and metoprolol. Amiodarone was later discontinued due to lethargy and intolerance. Event monitoring revealed frequent premature atrial contractions, premature ventricular contractions and brief nonsustained ventricular tachycardia (VT). In May 2018, she was put on dofetilide for rhythm control.
She continued to have increasing burden of symptomatic paroxysmal AF despite being on antiarrhythmic therapy. In October 2019, she underwent ablation for atrial fibrillation. Preprocedure transesophageal echocardiography showed normal LV function and absence of intracardiac thrombus. Patient underwent cryoablation (28 mm 2nd generation Arctic Front cryoballoon, Medtronic) of pulmonary veins to control AF. Procedure was performed under general anesthesia. She was in sinus rhythm at baseline. Patient had normal pulmonary venous anatomy. Firstly, left superior pulmonary vein was isolated then left inferior pulmonary vein (LIPV) was isolated. Baseline esophageal temperature (measured via single sensor, ES400-18) was 34.2 degree Celsius. During LIPV isolation, esophageal temperature declined to 30.1 degree Celsius. Lowest recorded cryoballoon temperature was - 47 degree Celsius. After 63 seconds of application freezing was stopped due to drop in esophageal temperature. There was concern for close proximity of esophagus to left veins and successive/cumulative freezing effect on esophagus. During thawing period patients heart rate decreased to 40 beats per minute (sinus bradycardia) and systolic blood pressure dropped down to 29 mm Hg (baseline of 109 mm Hg). Due to profound and rapid hypotension anesthesiologist used intravenous epinephrine up to 200 mcg. Her heart rate increased to 120 bpm and systolic pressure transiently increased to 220 mm Hg before normalizing. EKG (prior to epinephrine injection) revealed prominent ST elevation in inferior and V1 to V3 as well as ST depression in I and aVL followed by biphasic T-wave changes in inferior leads and precordial leads [figure 1A]. About 2 minutes after epinephrine, she had brief (<5 seconds) ventricular tachycardia (VT) which terminated by itself. EKG following VT termination showed more prominent (tombstone like) ST elevation in inferior and precordial leads [figure 1B]. By 10 minutes ST segments show significant resolution [figure 1C]. Subsequent ECG showed continued improvement ST segments with mild ST depression in inferior, lateral and high lateral leads with T wave inversion in precordial leads. Immediate transthoracic echocardiogram showed mild global hypokinesis with moderate hypokinesis of apex and no pericardial effusion. Left ventricular (LV) function was mildly reduced at 45%-50%. We continued with right sided pulmonary veins ablation, which was uneventful. Following ablation, bidirectional block was confirmed in all pulmonary veins.
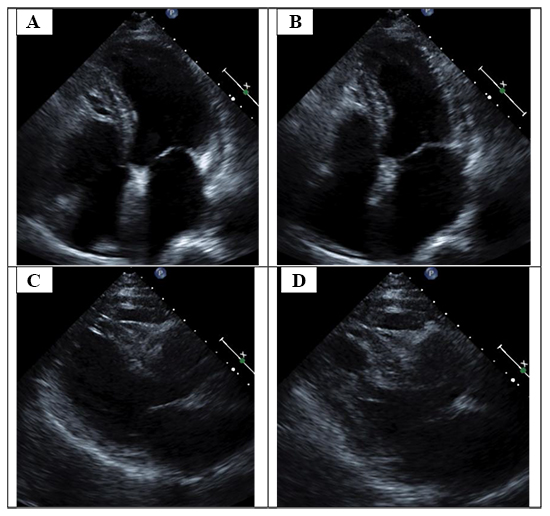
Post procedure EKG was done which revealed only borderline ST depression in inferior and high lateral leads, T wave inversion in precordial leads [figure 1D]. Patient denied chest pain, pressure or shortness of breath. Left heart catheterization was done within 24 hours revealed mild obstruction in the coronaries without any significant lesion and patent RCA stent. EKG at this time showed classical generalized wide T wave inversions in precordial lead and QT prolongation associated with TSC [figure 1E]. Echocardiogram revealed LVEF of 55% with hypokinetic distal apex [Figure 2A]-[Figure 2B]-[Figure 2C]-[Figure 2D]. These finding were consistent with recurrent TSC.
Figure 1A,B,C,D,E,F. Figure 1A- EKG showsprominent ST elevation in inferior and V1 to V3 as well as ST depression in I and aVL followed by biphasic T-wave changes in inferior leads and precordial leads. Figure 1B- EKG show prominent tomblike ST elevation in inferior leads and V1-V4, ST depression in I, aVL. This EKG is 8 minutes after figure 1A EKG and 2 minute after nonsustained VT. Figure 1C- EKG show significant resolution ST elevation in inferior and precordial leads (taken 10 minutes after figure 1A EKG). Figure 1D- EKG done in post-procedure recovery area revealed only borderline ST depression in inferior and high lateral leads, T wave inversion in precordial leads. Figure 1E- EKG (done 24 hours later) at this time showed classical generalized wide T wave inversions in precordial lead and QT prolongation associated with TSC. Figure IF- EKG done at 4 months show resolution of ST-T changes.
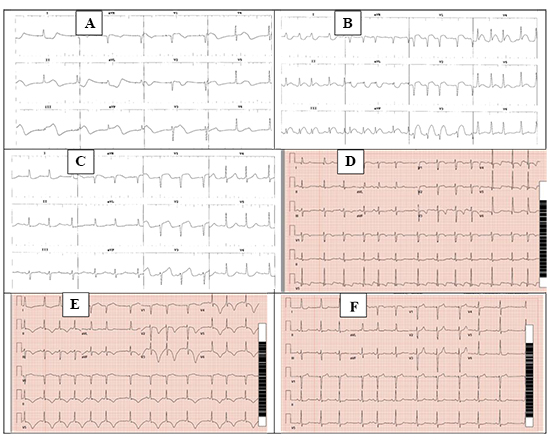
After the procedure, she stayed in sinus rhythm and her dofetilide was discontinued. She was continued on metoprolol, losartan, spironolactone and rivaroxaban. She had an echocardiogram 6 weeks after her cardiac ablation procedure which revealed an EF of 60% without any apical hypokinesis. Her ECG over next few days shows resolution of T wave inversion but continue to show biphasic T waves in precordial leads. T wave changes also resolved within 4 months [Figure 1F].
This case report shows that TSC can recur with stress of cryoablation for AF. TSC is often precipitated by emotional or physical stress. Recent reports have shown that TSC can also be associated with ablation procedure for arrhythmia, however only two reports of TSC related to cryoablation of AF are available.1, 2 One case reported on asymptomatic detection of EKG changes next day following pulmonary vein cryoablation for AF and cavotricuspid isthmus ablation. Second case describes TSC associated with pericardial tamponade and coronary artery injury. Our case is unique in multiple aspects. First, our report is the first care of recurrent TSC associated with cryoablation. Second, the detection of TSC followed immediately after pulmonary vein ablation and was not associated with coronary artery injury or tamponade. Third, this case report brings forth additional side effect of cryoablation when compared to radiofrequency, which in general is considered more potent in tissue damage. We also demonstrated the dramatic ECG changes in earlier stages of TSC. More importantly, our report allows readers to develop higher alertness for detection and management of TSC which can cause serious morbidity including death.3
Figure 2A,B,C,D. Figure 2A- End diastolic frame of 4-chamber view Figure 2B- End systolic frame of 4-chamber view shows relative hypokinesis of LV apex Figure 2C- End diastolic frame of parasternal long axis view Figure 2 D- End diastolic frame of parasternal long axis view (shortened) show apical ballooning and basal segment’s normal contractility
Cryoablation has been shown to preserve endothelial integrity and extracellular matrix.4 Cryoablation has also been shown to decrease procedure time and lower risk of moderate pulmonary vein stenosis compared to radiofrequency ablation.5-7 Despite relative safety of cryoablation, our case reveals possible complication of TSC arising from pulmonary vein ablation.
As to mechanism of TSC, two possible contenders are epinephrine use and autonomic dysfunction from ganglionic plexus (GP). Both alone or in combination could cause TSC. We hypothesize that GP ablation during cryoapplication precipitated significant bradycardia and hypotension to cause relative myocardial ischemia. Rapid use of intravenous epinephrine could have caused additional direct myocardial stunning or microvascular dysfunction. Focal ballooning is attributed to effect of catecholamine surge on LV myocardial wall segments with varying β-receptor densities; however, this theory is not supported by reports of different recurrent ballooning patterns.8 In our case, epinephrine use was followed by brief tachycardia, hypertension but its sole contribution to development of TSC remains suspect. Few reports of TSC associated with intravenous epinephrine are available.9-11 However, in all reports, five times higher dose of epinephrine compared to our patient (1000 mcg vs 200 mcg) was used. Additionally, a recent in-depth analysis of literature has questioned the direct causal relationship of epinephrine and TSC.12
An interesting angle as to possible development of TSC is role of GP ablation. Autonomic nervous system plays a significant role in initiating AF and atrial autonomic remodeling. GP are located close to pulmonary veins promote AF by predominantly parasympathetic action.13 Ablation of pulmonary veins via radiofrequency or cryoapplication can lead to at least partial GP ablation and therefore can have preventive effect on AF recurrence.14 Additionally, GP ablation can result into parasympathetic withdrawal or vagal denervation and therefore enhanced adrenergic tone.15, 16 However, cryoablation seem to have no greater effect than radiofrequency in terms of GP ablation.17 In our case, an intense hypotensive and bradycardic response was noted with LIPV cryoablation. If this response was followed by an intense sympathetic response from GP ablation which led to TSC, cannot be ascertained because patient also received a low dose intravenous epinephrine.
Other interesting fact of our case is recurrence of TSC. Recurrent TSC has been reported in up to 10% of cases with index TSC. Why some develop recurrent TSC while others develop possible immunity, is not well understood. Microcirculation dysfunction in addition to endothelial dysfunction is suspected to underlie the mechanism of recurrent TSC.18 Of note, cryoablation lesions cause almost no disruption of endothelial surface despite having acute effect of local myocardial necrosis.4
Our patient was treated with beta-blocker and angiotensin converting enzyme inhibitor along with her LV dysfunction and CAD therapy. Although, most patients are treated with beta-blockers and ACE inhibitors due to coexisting myocardial dysfunction, no randomized data is available showing efficacy of above therapy in preventing recurrent TSC.19
This case report suggests but does not prove conclusively that GP ablation related to pulmonary vein cryoablation lead to recurrence of TSC. A significant bradycardia and hypotension temporally related to thawing of cryoballoon and EKG changes suggest that excessive autonomic effect could have precipitated TSC as has been suggested by two reports. 16, 20 Patient also received epinephrine to raise blood pressure and patient had brief self-terminating VT that could be a significant stressor for development of TSC.
However, in this case relatively low dose (200 microgram) of epinephrine was used and VT lasted <5 seconds. It is possible that a relative low dose can result in significant myocardial tissue level and produce effects (BP and heart rate) as demonstrated in our patient. In our experience, use of vasopressor is very common in patients undergoing ablation under general anesthesia. Rare nature of TSC following ablation reduces likelihood of vasopressor as possible etiologic agent but does not exclude it. Transient ST elevation during ablation has also been attributed to possible parasympathetic nerve damage during transseptal puncture, air embolism or coronary artery spasm. In this case, ST changes happened at least 20 minutes after transseptal puncture. We use continuous intravenous flushing of sheaths and take due diligence in avoiding air embolism. Air embolism often affects right coronary artery and is associated with AV block.
Generalized ST-T changes in ECG and absence of AV block reduces possibility of air embolism as an etiology. Coronary artery spasm is also unlikely because of posterior nature of left inferior pulmonary vein and absence of abnormal anatomy in this patient.
This case report describes recurrence of TSC associated with pulmonary vein cryoablation for AF. Readers should also appreciate that recurrent TSC could be associated with serious morbidity including death. Therefore, recognition and management of recurrent TSC is warranted.