Atrial Fibrillation After Lung Transplantation:
Incidence, Predictors and Long-Term Implications
Santiago Garcia MD1,3, Mariana Canoniero MD 1, Srinivasan Sattiraju MD1, Lin Y. Chen MD1, Wayne Adkisson MD1, Marshall Hertz MD2, David G. Benditt MD1
1University of Minnesota, Department of Medicine, Division of Cardiovascular Medicine. Minneapolis, MN.2University of Minnesota, Department of Medicine, Division of Pulmonary and Critical Care Medicine. Minneapolis, MN.3Minneapolis VA Medical Center. Minneapolis, MN.
Little is known about the frequency of, risk factors predisposing to, and long-term impact of post-operative atrial fibrillation (AF) after lung transplantation.
A prospectively collected registry of 167 consecutive patients who underwent single or bilateral lung transplantation at the University of Minnesota Medical Center from January 1st, 2004 to December 30th, 2008 was reviewed. Post-operative AF was confirmed by review of electrocardiograms by two cardiologists. Kaplan-Meier survival curves were constructed to determine the impact of new onset AF on long-term survival.
The mean age (±SD) of the population was 55 ± 11 years and 52% were male. A total of 48 patients (28%) developed AF in the postoperative period. Predictors of postoperative AF in multivariate analysis included: age (per decade) Odds Ratio (OR): 1.61, 95% confidence interval (CI) 1.10-2.34, p=0.01, postoperative thromboembolic disease OR: 9.73 (95% CI: 2.16-43.81, p<0.01, and postoperative pericarditis OR: 3.57, (95% CI: 1.38-9.22, p < 0.01). Of the 48 patients who developed post-operative AF, 41 were discharged in sinus rhythm (SR). Survival among patients who were discharged in AF was significantly lower when compared to patients discharged in SR (HR: 0.08; 0.01-0.43, p<0.05).
Postoperative AF is common after lung transplant. Increased age, postoperative thromboembolic disease, and pericarditis are independent predictors of postoperative AF. Persistence of AF at the time of discharge is an identifier of decreased survival.
Correspondence to: Santiago Garcia, MD, One Veterans Drive (111-C), Minneapolis, MN (55417).
Lung transplantation is an accepted treatment modality for selected patients with end-stage lung disease.1 Each year in the U.S. 1.400-1.600 patients undergo single or double lung transplantation with an overall expected 5-year survival of 50%.2-3 Lung transplant recipients are at risk of developing serious complications in the postoperative period including graft failure, pulmonary edema, infections, nerve injury and atrial tachyarrhythmias.4-8
Atrial fibrillation is among the most common complications after lung transplantation with a reported incidence of 20%-39%. Its occurrence has been associated with increased hospital stay and in-hospital mortality in some series.9 The mechanisms leading to atrial fibrillation in this setting are likely to be multifactorial but remain poorly understood.9-11 Post-operative atrial fibrillation is generally transient and at hospital discharge normal sinus rhythm has been restored in the vast majority of patients. The long-term implications of persistent atrial fibrillation have never adequately been studied.
The purpose of this investigation was to assess the frequency of, risk factors predisposing to, management strategies, and long-term impact of post-operative atrial fibrillation after lung transplantation.
The study cohort consisted of 167 consecutive patients with end-stage lung disease who underwent lung transplantation at the University of Minnesota Fairview Medical Center from January 1st 2004 through December 30th 2008.
A prospectively collected registry was reviewed for demographic and clinical information. Unique patient identifiers were obtained and used to link the registry with electronic medical records and an electrocardiographic database. When appropriate the social security death index was used to ascertain vital status during long-term follow up. Two independent cardiologists reviewed all electrocardiograms.
Univariate analysis was carried out to identify variables that were significantly associated with post-operative atrial fibrillation. The following variables were included in univariate analysis: Demographics: age, gender, weight; Co-morbid conditions: diabetes mellitus, arterial hypertension, coronary artery disease, obstructive sleep apnea, chronic kidney disease, and prior atrial fibrillation; Post-operative complications: myocardial infarction, pericarditis, sepsis, ≥ 1 vasoactive drugs, thromoboembolic disease, allograft failure Echocardiographic variables: left atria enlargement (>40 mm).
Using univariate predictors that showed a possible association with the outcome of interest (p<0.1) a logistic regression model with backward elimination was developed. In this model variables with p > 0.1 were removed and variables with p <0.05 were entered. Kaplan-Meier product-limit estimates were used to generate survival curves and the log-rank test was used to evaluate survival differences.
Continuous variables demonstrating a normal distribution are expressed as mean ± standard deviation (SD) and discrete variables are presented as frequencies and percentages. When appropriate, continuous variables were compared between the two groups using the non-paired Student’s t test for normally distributed data and the Mann-Whitney U test for non-normally distributed data. Proportions were compared with the Chi square test. Statistical significance was defined as a two-tailed p value less than 0.05. Medcalc ® for Windows® version 11.3 (Mariakerke, Belgium) was used to perform the statistical analysis.
Definitions of co-morbid conditions were derived from the American College of Cardiology Task Force on clinical data standards when appropriate.12 Post-operative complications were identified from the medical records and defined by the clinician treating the patient. Whenever possible, specific clinical diagnoses listed in the medical record (i.e. pulmonary embolism) were confirmed with objective data (i.e. CT angiography) by the investigator abstracting the data. All cases of myocardial infarction were confirmed by an elevated troponin T above the 99th percentile with ischemic electrocardiographic changes. The Institutional Review Board of the University of Minnesota approved the study (Number: 0805E33181).
Of the 167 patients who underwent lung transplantation during the study period, 62 (36.5%) received a bilateral and 104 (61%) a single lung transplant. One patient received a combined heart/lung transplant and one a partial lobe.
The mean age (±SD) of the recipients was 51 years (±11) and 52% were male. The mean age of the donors was 34±15 years.
Table 1. Baseline characteristics of the study cohort (n=168)
| Characteristic |
Value |
| Recipient age ±SD (years) |
51 ± 11 |
| Donor age ± SD (years) |
34 ± 15 |
| Weight ± SD (Kg) |
74 ± 20 |
| Height ± SD (cm) |
|
|
170 ± 9 |
| Male Gender (%) |
52% |
| Primary Diagnosis: |
|
| Alpha-1 antitrypsin deficiency (%) |
8% |
| Cystic fibrosis (%) |
18% |
| Emphysema/chronic obstructive pulmonary disease (%) |
26% |
| Idiopathic pulmonary fibrosis (%) |
28% |
| Others (%) |
20% |
| Co-morbid conditions: |
|
| Arterial hypertension (%) |
45/168 (27%) |
| Diabetes mellitus (%) |
28/168 (17%) |
| Coronary artery disease (%) |
12/168 (7%) |
| Stroke (%) |
1/168 (1%) |
| History of atrial fibrillation (%) |
8/168 (5%) |
| Obstructive sleep apnea (%) |
4/168 (2%) |
| Chronic kidney disease (%) |
13/168 (8%) |
| Echocardiographic variables (n=116): |
|
| Left atrial size (mm) -mean ± SD |
35±8 |
| Right ventricular systolic pressure (mmHg) - mean ± SD |
41± 19 |
| Ejection fraction (%) ± SD |
57± 7 |
The four most common indications for lung transplantation included: idiopathic pulmonary fibrosis (28%), emphysema/chronic obstructive pulmonary disease (26%), cystic fibrosis (18%), and alpha-1 antitrypsin deficiency (8%). Other baseline characteristics of the cohort are described in Table 1.
In the post-operative period (within 30 days), 59 patients developed supraventricular tachyarrhythmias (35%). The most common arrhythmias were atrial fibrillation (n=48) and atrial flutter (n=10). The overall incidence of new post-operative atrial fibrillation was 29%. Atrial fibrillation developed at a mean of 4 ± 3 days after the index surgical intervention.
Uni- and multivariate predictors of post-operative atrial fibrillation are presented in Table 2. Univariate predictors included age, prior atrial fibrilla tion, post-operative pericarditis and post-operative thromboembolic disease. When these four variables were entered in a logistic regression model with backward elimination only three remained significant predictors of post-operative atrial fibrillation: age (for incremental increases in age expressed in decades) odds ratio (OR): 1.61, 95% confidence interval (95% CI) 1.10-2.34, p=0.01, post-operative pericarditis OR: 3.57 (95% CI: 1.38-9.22), p< 0.01, and post-operative thromboembolic complications OR: 9.73 (95% CI: 2.16-43.81), p < 0.01. The incidence of post-operative pericarditis and thromboembolic complications were 13% (n=22) and 6% (n=10), respectively.
Figure 1 Kaplan-Meier survival curve for lung-transplant patients with and without post-operative atrial fibrillation
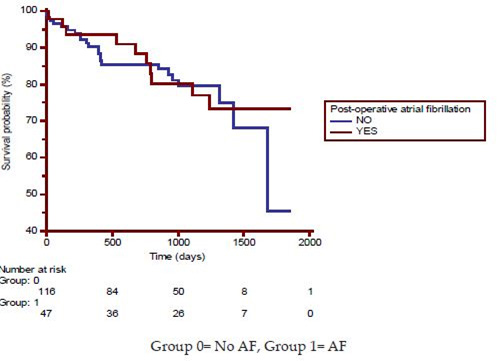
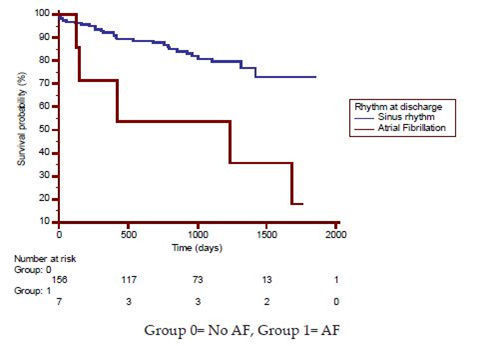
Figure 2 Kaplan-Meier survival curve for lung-transplant patients according to heart rhythm at discharge
The management of post-operative atrial fibrillation involved medical therapy or electrical cardioversion in the vast majority of patients prior to discharge (44/48). Utilized therapies included: amiodarone (n=27, 61%), calcium-antagonists (n=4, 9%), beta-blockers (n=7, 16%), and electrical cardioversion (n=5, 11%). Anticoagulation was initiated in the hospital in 19 patients (43%), 13 patients received no antithrombotic therapy (29%), and 12 patients received aspirin monotherapy (27%).
Short- and long-term survival was unaffected by the presence of post-operative atrial fibrillation (Hazard ratio (HR): 1.10, 95 % CI: 0.52-2.29, p=0.78) (Figure 1). Of the 48 patients who developed post-operative atrial fibrillation, 41 were discharged in sinus rhythm. When compared to patients who were discharged in atrial fibrillation, patients discharged in normal sinus rhythm showed better long-term survival (HR: 0.08; 0.01-0.43, p<0.05) (Figure 2).
The main findings of this observational study may be summarized as follows: 1) atrial fibrillation affects one third of patients undergoing lung transplantation, 2) the incidence of post-operative atrial fibrillation tends to increase with age, 3) the development of post-operative pericarditis and thromboembolic complications (DVT/PE) are strongly associated with post-operative atrial fibrillation, 4) persistence of atrial fibrillation beyond the post-operative period, although rare, is associated with decreased survival.
Our findings are in agreement with two previously reported observational studies.9,13 Nielsen et al. reported on the outcomes of 200 consecutive patients undergoing lung transplantation at Duke University Medical Center from from June 2002 to August 2008. In this series, 39% of patients developed atrial fibrillation, with a mean onset of 3.8 days. In addition to older age (> 50 years), coronary artery disease, idiopathic pulmonary fibrosis, left atrial enlargement, and number of postoperative vasopressors were found to be independent predictors of post-operative atrial fibrillation. Unlike our study, atrial fibrillation significantly increased the risk of in-hospital (OR=5.7, p<0.01) as well as long-term mortality in this cohort. It should be noted that Nilesen’s study did not distinguish between the majority of patients who converted to sinus rhythm during the index hospital admission and the small fraction of patients who were discharged in atrial fibrillation. In our cohort only patients with persistent atrial fibrillation at the time of hospital discharge had increased long-term mortality.
Table 2. Univariate and multivariate predictors of post-operative atrial fibrillation.
|
Univariate Predictors |
Multivariate Predictors |
|
| Variable |
B coefficient |
P value |
B coefficient |
P value |
OR (95% CI) |
|
|
Demographics |
|
|
|
| Age (each increase of 1 decade) |
0.14 |
0.06 |
0.46 |
0.01 |
1.61 (1.10-2.34) |
| Male gender |
0.08 |
0.28 |
-- |
-- |
-- |
| Weight (≥ mean) |
0.03 |
0.82 |
-- |
-- |
-- |
|
|
Co-morbid conditions |
|
|
|
| Diabetes mellitus |
0.07 |
0.34 |
-- |
-- |
-- |
| Arterial hypertension |
-0.07 |
0.92 |
-- |
-- |
-- |
| CAD |
-0.74 |
0.34 |
-- |
-- |
-- |
| OSA |
0.07 |
0.34 |
-- |
-- |
-- |
| CKD |
0.01 |
0.86 |
-- |
-- |
-- |
| Prior atrial fibrillation |
0.17 |
0.02 |
0.12 |
NS |
-- |
|
|
|
Post-operative complications |
|
|
| Myocardial infarction |
0.09 |
0.21 |
-- |
-- |
-- |
| Pericarditis |
0.22 |
<0.01 |
1.27 |
< 0.01 |
3.57 (1.38-9.22) |
| Sepsis |
0.01 |
1.00 |
-- |
-- |
-- |
| ≥ 1vasoactive drugs |
0.10 |
0.19 |
-- |
-- |
-- |
| Thromboembolic disease (DVT/PE) |
0.17 |
0.02 |
2.27 |
< 0.01 |
9.73 (2.16-43.81) |
| Graft failure |
-0.03 |
0.66 |
-- |
-- |
-- |
|
|
|
Echocardiographic Variables |
|
|
| LA enlargement (> 40 mm) |
0.01 |
0.94 |
-- |
-- |
-- |
Additionally, in a more contemporary cohort of patients followed at The Cleveland Clinic after lung transplantation, post-operative atrial fibrillation did not have an effect on short- or long-term survival.13 Mason et al.13 analyzed risk factors, management strategies, and outcomes of 333 consecutive patients who developed atrial fibrillation after lung transplantation. The incidence of post-operative atrial fibrillation in this series was 20%, with a peak incidence 2 days after operation. Similarly to our study, older age was an independent predictor of post-operative atrial fibrillation along with primary pulmonary hypertension and extreme weight. However, in our Researchcohort neither weight nor primary pulmonary hypertension was an independent predictor of atrial fibrillation. Potential explanation for these differences are the relative low frequency of primary pulmonary hypertension as an indication for lung transplantation in our cohort (2%) and the loss of statistical significance of a relatively weak predictor such as weight when other variables, not included in the former analysis,13 were entered in the model such as post-operative pericarditis and thromboembolic complications.
Table 3. Comorbidities and causes of death among patients with persistent atrial fibrillation at discharge who died during follow up.
| Patient |
Age |
Gender |
Indication for lung transplant |
LA size (mm) |
Previous heart disease |
Cause of death |
| #1 |
62 |
Male |
Pulmonary fibrosis |
41 |
No |
Myocardial infarction |
| #2 |
44 |
Male |
Cystic fibrosis |
39 |
-Prior atrial fibrillation
-Diabetes |
Bacterial infection |
| #3 |
50 |
Female |
Obliterative bronchiolitis |
46 |
- Prior atrial fibrillation
-Hypertension |
Unspecified heart disease |
| #4 |
63 |
Female |
Pulmonary fibrosis |
45 |
- Hypertension |
Alveolar hemorrhage |
| #5 |
59 |
Male |
Cystic fibrosis |
37 |
No |
Infection |
| #6 |
43 |
Male |
Cystic fibrosis |
37 |
No |
Bacterial infection |
| #7 |
52 |
Male |
ASD with Eissenmenger physiology |
55 |
- Shunt |
Stroke |
Post-operative pericaridits has been linked to atrial fibrillation after cardiac surgery.14 Pericarditis may cause atrial epicardial inflammatory injury and serve as a substrate for atrial fibrillation. For example, epicardial implantable cardioverter-defibrillator (ICD) implantation results in significantly more cases (9%) of post-operative atrial fibrillation than does transvenous ICD implantation (1%). 15Additionally, the risk of post-operative pericarditis during non-cardiac thoracic surgery appears to increase when the pericardium is manipulated surgically.16 In some series, however, pericarditis was not found to be predictive of post-operative atrial fibrillation.17 The association of atrial fibrillation and pulmonary embolism has been well recognized.18 Atrial fibrillation not only can be a sign of pulmonary embolism but it may also lead to pulmonary or systemic embolization when accompanied by intracavitary thrombus.19-20 When atrial fibrillation develops in the context of pulmonary embolism it is thought to be secondary to acute right-sided pressure overload with stretching of the right atrium, which is usually accompanied and aggravated by tricuspid regurgitation.21-22
The finding of increased mortality among patients who leave the hospital in atrial fibrillation vs. normal sinus rhythm is hypothesis generating and deserves further study. It is plausible that this subset of patients in whom therapies failed, or were not considered, has a different substrate to develop and maintain atrial fibrillation such as subclinical cardiac dysfunction, infection or allograft rejection.
A detailed analysis of the causes of death Table 3 shows that approximately 50% of patients died from infectious causes. This would suggest that the association between atrial fibrillation and mortality might be spurious and not causal. Given the lack of a demonstrable survival benefit in randomized clinical trials with a rhythm-control strategy,23 it is conceivable that unmeasured confounders could account for the observed mortality differences rather than being a direct effect of a rhythm-control strategy.
The introduction of catheter-based pulmonary Researchvein (PV) isolation procedures to terminate atrial fibrillation has sparked renewed interest in lung transplant recipients, as they constitute a “surgical model” of pulmonary vein isolation.11 Single and double lung transplant surgery involves a ‘cut and sew’ PV antral isolation analogous to a catheter-based approach. Despite these theoretical considerations, atrial fibrillation occurs with equal frequency after lung transplantation and open-heart surgery (20-39%), and at a much higher frequency than heart transplantation (4%).10 This observation suggests a more prominent role of cardiac denervation in the pathogenesis of atrial fibrillation after thoracic transplant surgery and a less prominent role of pulmonary vein isolation, which is also performed during heart transplant.
The study has intrinsic limitations owing to the type of design (i.e. single center, retrospective) and limited power due to small sample size in statistical terms. Therefore, the findings of this study should be considered hypothesis generating rather than confirmatory.
After lung transplantation atrial fibrillation is a common post-operative complication affecting about one third of patients. Increased age, postoperative thromboembolic disease, and pericarditis are independent predictors of post-operative atrial fibrillation. Persistence of atrial fibrillation at the time of discharge is an identifier of decreased survival.