AF is the most common sustained cardiac arrhythmia, occurring in 1 – 2% of the general population. In the majority of patients there appears to be an inexorable progression of AF to persistent or permanent forms, associated with further development of the disease that may underlie the arrhythmia.1
The rate of AF recurrence is 10% in the first year after the initial diagnosis (25–50% in the first month after restoration of sinus rhythm) and about 5% per annum thereafter. Co-morbidities and age significantly accelerate both the progression of AF and the development of complications.1 Moreover, it was reported that only about the 30% of patients with recurrences of any type of AF at any time were symptomatic.2 Factors that predispose to AF recurrence are age, AF duration before restoration of sinus rhythm, number of previous recurrences, an increased left atrial (LA) size or reduced LA function, and the presence of coronary heart disease or pulmonary or mitral valve disease. Atrial ectopic beats with a long – short sequence, faster heart rates, and variations in atrial conduction increase the risk of AF recurrence.1 As well known, a complete echocardiographic exam of a patient with AF, in order to decide a therapeutical approach, includes measurements of LV systolic function and dimensions, valvulopathiesdegree and LA dimensions. However echocardiographic parameters to clearly predict AF recurrence are not known. LV diastolic dysfunction degree has been associated with new-onset AF3 and in the last few years many new parameters to evaluate diastolic function were introduced and validated, even in patients with AF.4,5
Aim of this review was to summarize echocardiographic parameters, focusing on new tools, to evaluate patients with AF and to explore the role of echocardiographic evaluation to predict recurrence of the arrhythmia.
Standard Echocardiography
In daily practice a standard echocardiogram was performed in patients with AF or with history of AF. LA enlargement has been identified as a risk factor for new onset AF6 than for AF recurrence.
Increased left atrial volume (LAV) is a well known indicator of chronic diastolic dysfunction. Commonly encountered AF in older patients with cardiovascular disease is preceded by atrial enlargement and increased left ventricular filling pressures.7 In patients who underwent radio frequency catheter ablation (RFCA) for lone AF, LA dimensions are associated with arrhythmia recurrence. In the study of Hussein et al,8 LA area, LV ejection fraction and pre-procedural BNP (Brain Natriuretic Peptide) were independently associated with AF recurrence ain the 24 months follow up period in patients who underwent successful RFCA. It is well known that BNP levels are closely related to LA and LV dimensions. Patients with AF recurrence had a significantly larger LA size, increased E-wave (early wave) velocity, and an increased E/e' ratio (average between lateral and septal wall) compared to patients who maintained SR.9 However, a more accurate estimation of LA dimensions must include evaluation of LAV. 2D LAV, in facts, represents a more comprehensive evaluation of the 'true' LA size and it may improve the identification of patients with a high likelihood of maintaining of sinus rhythm. In a recent work by Marchese et al10 411 patients who underwent successful cardioversion for AF were scheduled for a follow-up of at least 6 months in order to assess rate of recurrence and value of 2D indexed LAV (iLAV) as predictor of AF recurrence. About 250 patients (60.8%) developed AF recurrence after a median follow-up of 345 days. Patients with AF recurrence had significantly greater iLAV than patients without AF recurrence. In a multivariable model, each ml/m2 increase in iLAV was independently associated with a 21% increase in the risk of AF recurrence. A value of iLAV of 33.5 ml/m2 was characterized by an 83% sensitivity and 76% specificity to predict AF recurrence. These findings were confirmed in patients undergoing RFCA.11 Significantly dilated atria are generally thought to be associated with a high degree of atrial remodeling which limits the efficacy of RFCA.11 LA volumes can be measured at 3 points: 1) in ventricular systole just before mitral valve opening (LAV max); 2) before active atrial contraction volume at P-wave onset on ECG (LAV before P) ; and 3) minimal LA volume after mitral valve closure (LAV min). LA passive (LA PEF: LAV max- LAV before P/LAV max) and active emptying fraction (LA AEF: LAV before P- LAV min/LAV before P) can be used as parameters of atrial function. LA PEF is an index of passive component of LA pump function, while LA AEF of active component.12 LA total emptying fraction (LAV max- LAV min/LAV max), that is expression of either passive and active component of LA pump function, was proposed in literature as predictor of first episode of AF or atrial flutter. It was demonstrated that, in patients over 65 years old, this parameter was associated with risk for first AF or atrial flutter after adjusting for baseline clinical risk factors, left ventricular ejection fraction, diastolic function grade, and LA volume.13 However, an important limit of these parameters is that they are derivative parameters, and thus aincorrect detection of 2D LA volumes could potentially determine a modification of emptying fractions. Atrial ejection force and la kinetic energy14 can be assessed non invasively by combined two-dimensional imaging and A wave measurement, obtained by Doppler echocardiography (mitral annulus dimension in 4 chamber apical view for LA ejection force and LA stroke volume for LA kinetic energy, respectively) . These parameters have been proposed in the last decades as direct measurements of LA mechanics after CVE cardiovascular events (CVE) and in chronic heart failure.15,16 However their clinical significance is poorly defined.
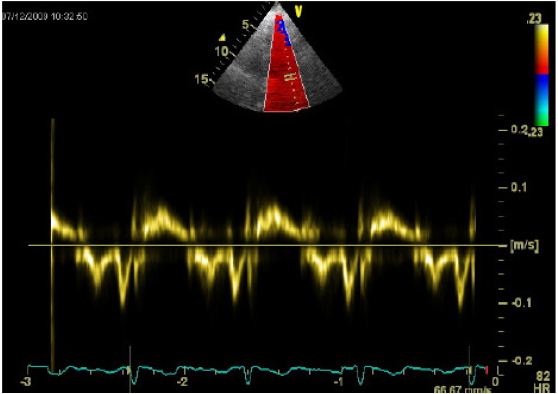
The ratio of early diastolic transmitral flow velocity (E) to early diastolic mitral annular velocity (e’), a tissue Doppler imaging derived index of LV diastolic function, allows for the noninvasive assessment of left ventricular filling pressure and estimation of atrial pressure.17 The most recent guidelines for echocardiographic evaluation of diastolic function indicate E/e’ ratio (average between lateral and septal wall) as a key parameter in the estimation of degree of diastolic dysfunction Fig. 1. E/e’ ratio has been well validated in the evaluation of outcome in patients with AF.18 The role of E/e’ ratio as predictor of AF recurrence after successful electrical cardioversion was investigated in our previous study. We evaluated patients with persistent non valvular AF ,who underwent electrical cardioversion. After 1 year follow up 43% of patients showed AF recurrence. E/e’ ratio was an independent predictor of even early and late AF recurrence. In our study values of 5.6, 8.1, and 10.5 for E/e' corresponded to estimated 25%, 50%, and 75% risks, respectively.19 These data are confirmed in patients undergoing RFCA for AF. Li et al20 enrolled 103 patients who underwent RFCA for symptomatic non- valvular persistent or paroxysmal AF. The E/e’ ratio measured before ablation was independent predictor of early AF recurrence (3 months follow up). A cutoff value of 11.2 for the E/e’ measured before ablation was associated with a sensitivity of 80.8% and specificity of 81.8% for AF recurrence. E/e’ measured in sinus rhythm 1 day after ablation had an even better predictive power with a sensitivity of 88.5 % and a specificity of 87%. Similar results were obtained in patients undergoing RFCA.21,22 Patients with diastolic dysfunction had a lower mean LA voltage even after adjusting for hypertension and the age and multivariate analysis indicated diastolic dysfunction and LA voltage as independent predictors of recurrence. Authors hypothesized that diastolic dysfunction results in a chronic diastolic atrial pressure overload, and subsequent LA remodeling, and that decrease in LA voltage was expression of early atrial remodeling.22 Low (< 0.5 mV) or absent (<0.05 mV) electrographic recording, measured with extensive voltage mapping of the left atrium (LA) are defined as "scarring". It was reported that presence and extension of LA scaring before RFCA is related with recurrence of arrhythmia.23
Figure 1. Tissue Doppler measurements on LV lateral wall
Strain and strain rate are parameters that can be obtained offline, with dedicated softwares. Strain rate (SR) is defined as the local rate of deformation of a tissue and strain the total amount of local deformation. Tissue Doppler imaging (TDI) data can be acquired during a standard echocardiogram. Strain and SR are then performed with offline analysis. Peak regional and global longitudinal strain are measured at the end of LV ejection, while LA SR is measured as peak systolic, during early and late diastolic (atrial contraction) LV filling. In patients with AF, late diastolic SR is absent. Di Salvo et al24 measured TDI strain and SR in mid segment of LA inferior wall in 65 consecutive patients with lone AF before electrical cardioversion. In the subgroup of patients with AF recurrence atrial myocardial properties assessed by SR and strain were significantly reduced respect to patients who remained in sinus rhythm after nine months. In the study of Wang and colleagues25 LA transverse diameter was significantly larger and atrial early diastolic deformation was significantly lower in patients who reverted to AF within 4 weeks after electrical cardioversion for persistent AF. These parameters were independent predictors of failure of the procedure and their combination in a prediction model improve sensitivity and specificity to predict the likelihood of maintenance of sinus rhythm. Recently, strain and SR measurements have been measured with speckle tracking echocardiography (figure 2 and 3).
Figure 2. LA atrial strain curves by speckle tracking echocardiography. PALS: peak of atrial longitudinal strain.
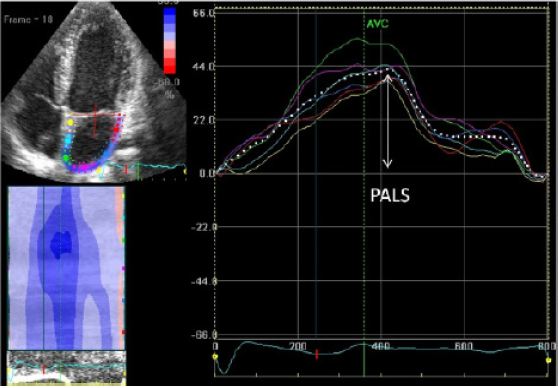
Figure 3. LA strain rate by speckle-tracking echocardiography
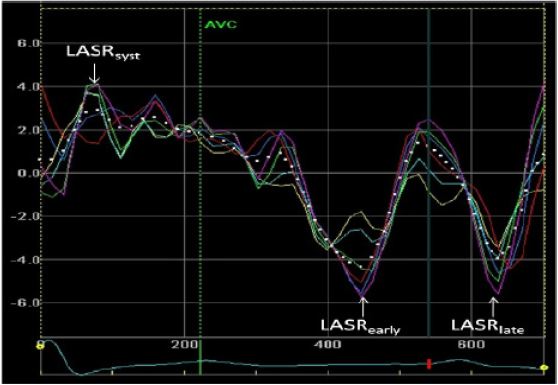
Two-dimensional strain imaging is an echocardiographic technique that uses standard B-mode images for speckle tracking analysis. The displacement of a speckled pattern is considered to follow myocardial movement. For speckle tracking analysis of LA chamber, apical four- and two-chamber views images are obtained using conventional two-dimensional gray scale echocardiography, during breath hold with a stable ECG recording. In contrast to Doppler-derived parameters, speckle tracking has the advantage of being angle-independent, and to be less affected by reverberations, side lobes and drop out artifacts.26 Nonetheless, intrinsic limitations of speckle tracking include strict frame rate dependency, potential errors in epicardial/endocardial border tracing in subjects with suboptimal image quality, and need for an appropriate learning curve to achieve adequate experience in using analysis software.26 Atrial myocardial deformation properties have been investigated in several clinical settings.27–29 It was reported that in patients with mitral regurgitation and clinical history of paroxysmal AF, LA global strain is significantly reduced.30 In patients who underwent cardiac surgery it is well known that postoperative AF is an important and relatively common complication, occurring in up to 65% of patients.31 In 70 patients undergoing coronary artery bypass grafting, in sinus rhythm at the time of surgery, preoperative LA strain and strain rate by speckle tracking were significantly decreased in patients who developed postoperative AF after 1 week follow-up.32 Hwang et al33 analyzed LA global longitudinal strain in 40 patients with paroxysmal AF who underwent RFCA compared with 40 age- and gender-matched healthy control subjects. Global strain and systolic SR in all eight segments, and its average values, were significantly reduced in AF patients compared to controls. During 9 months of follow-up after RFCA AF recurrence was associated with gender, LA volume index, and global strain. Even in the more recent study by Mirza et al34, reduction of LA strain indices were independent predictors of AF recurrence after RFCA. LA strain was measured before RFCA (in sinus rhythm) and patients were followed up for 3 months. In patients that had AF recurrence (46%), LA global strain and SR were significantly reduced and particularly LA strain of lateral wall, that emerged as independent predictor of AF recurrence, even in patients with paroxysmal AF. Interestingly, in this study both groups had similar 2D echocardiographic and Doppler features, including LA volumes, LV mass index, LVEF, and other parameters of systolic and diastolic function. It is possible that in these patients, despite similar atrial dimensions, there is greater chamber stiffness and thus a reduced atrial reservoir function, as indicated by depressed global strain and SR. In the study by Hammerstingl et al,35 LA radial and longitudinal strain were obtained in 103 consecutive patients with paroxysmal or persistent AF before RFCA, to predict AF recurrence rate. In Respect to matched controls, AF patients before RFCA had a reduction in global LA deformation capabilities, assessed by strain indices. Machino-Ohtsuka T et al36 measured LA stiffness as ratio of difference between LA maximum and minimum invasive pressure to peak of LA strain obtained with speckle tracking echocardiography. This parameter was obtained in 155 patients who underwent RFCA. Authors aimed to demonstrate also that a similar non invasive parameter could be easily calculated with a combination of the atrial filling pressure (i.e. E/e’ ratio) and LA strain. Patients with recurrent AF had a significantly higher LA stiffness index before ablation. The invasive LA stiffness index was correlated with the BNP, PIIIP (a collagen synthesis marker), E/e’ ratio, and LA dilatation, which are markers of LV diastolic dysfunction. Authors hypothesis was that this parameter could "read" structural and functional remodeling of LA that, in turn, might account for greater risk of AF recurrence. Hirose et al37 prospectively observed a cohort of 580 adults without a history of atrial arrhythmias. 32 of them developed an episode of AF during a follow up of 28 months. In this subgroup LA active ejection fraction, was an independent predictor of new onset AF, better than LA size. Authors’ concluded that this parameter, that reflects atrial booster pump function, is associated with LA functional remodeling stronger than LA size Fig. 2.
2 D strain and strain rate measurements, if adequately obtained, could represent a valid tool to detect early modifications in LA substrate. However, multicenter studies are needed to define a unique method of measurements and reference values.
Three-Dimensional Echocardiograpy
Recently, a more accurate evaluation of LAV was introduced throughout 3 D measurements of LA size. The available three-dimensional imaging modalities include magnetic resonance imaging, and three-dimensional echoJournal cardiography. These methods are useful to a better assessment of LA size, morphology and substrate, which may significantly improve prediction of successful RFCA for AF, although limited by the necessity of sinus rhythm.38,39 Fig. 3